A comparison study of blood lactate and lactate clearance with SNAP II score as predictors of outcome in sick neonates
Abstract
Introduction: Necessity of longer stay in NICU reinforces the need for more sensible and specific parameter to evaluate the length of stay and outcome. In order to improve the clinical outcomes in sick neonates, it is crucial to obtain early recognition of those who are at risk of morbidity and mortality and to optimize the clinical decision making in a timely manner and to counsel the parents.
Aims & Objectives: This study was designed to compare and obtain best predictor of outcome irrespective of diagnosis.
Materials and Methods: The study was “prospective observational” study, conducted at NICU over 188 sick neonates of Pragna hospitals, Hyderabad in the period of October 2013 to september2015.
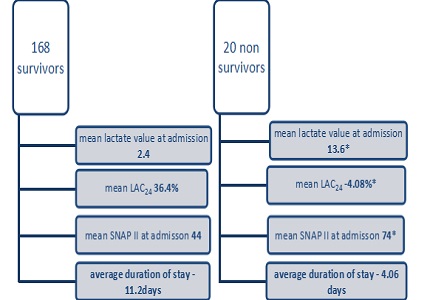
Results: Among 188 sick neonates 20 were non survivors, and 168 survived. There was significant correlation between high lactate at admission, low LAC24 of less than 30% and high SNAP II score at admission with mortality among sick neonates. Neonates with LAC24 of < 30% had significantly higher requirement of oxygen (p-0.00*), fluid support (p-0.00*), ionotropes(p-0.0002**), ventilator support(p-0.0015**) and length of stay(p-0.004*) than with LAC24> 60%. There were 23 neonates with initial lactate of more than 9mmol/dl. 6 out of 23 had LAC24 of less than 30%. 4 out of 6 had LAC48 of more than 30% yet, all 6 neonates had prolonged duration of stay with an average of 15.3 days. Neonates with high SNAP II score at admission of more than 60 had higher requirement ionotrope, and ventilator support. The area under curve (ROC) revealed poor correlation with overall morbidity.
Conclusion: Lactate clearance value of less than 20.4% at 24 hours of admission could be useful to predict the adverse outcome with significant need for mechanical ventilation, higher oxygen, fluid and inotrope support and prolonged stay in sick neonates irrespective of diagnosis
Downloads
References
2. The international Neonatal Network. The CRIB (Clinical Risk Index for Babies) score: a tool for assessing initial neonatal risk and comparing performance of neonatal intensive care units. Lancet 1993; 342:193-198.
3. Pollack MM, Koch MA, Bartel DA, Rapoport I, Dhanireddy R, El-Mohandes AA, Harkavy K, Subramanian KN. A comparison of neonatal mortality risk prediction models in very low birth weight infants. Pediatrics. 2000 May;105(5):1051-7.
4. Karimova A, Pinsky DJ. The endothelial response to oxygen deprivation: biology and clinical implications. Intensive Care Med. 2001 Jan;27(1):19-31.
5. Hack CE, Zeerleder S. The endothelium in sepsis: source of and a target for inflammation. Crit Care Med. 2001 Jul;29(7 Suppl):S21-7. [PubMed]
6. Munde A, Kumar N, Beri RS, Puliyel JM. Lactate clearance as a marker of mortality in pediatric intensive care unit. Indian Pediatr. 2014 Jul;51(7):565-7. [PubMed]
7. RE Musson, SJ Clark, R Kachroo, S Didier and M Smith. Arch Dis Child Fetal Neonatal Ed 2013 98: A61, doi: 10.1136.
8. Kana Ram, Urmila Jhamb, Vinod K. Gupta. Indian Journal of Critical Care Medicine :2011; 15: 2. [PubMed]
9. Deshpande SA, Platt MP. Association between blood lactate and acid-base status and mortality in ventilated babies. Arch Dis Child Fetal Neonatal Ed. 1997 Jan;76(1):F15-20. [PubMed]
10. Marty P, Roquilly A, Vallée F, Luzi A, Ferré F, Fourcade O, Asehnoune K, Minville V. Lactate clearance for death prediction in severe sepsis or septic shock patients during the first 24 hours in Intensive Care Unit: an observational study. Ann Intensive Care. 2013 Feb 12;3(1):3. doi: 10.1186/2110-5820-3-3.
11. Jones AE, Shapiro NI, Trzeciak S, Arnold RC, Claremont HA, and Kline JA: Lactate clearance vs central venous oxygen saturation as goals of early sepsis therapy: a randomized clinical trial. JAMA 2010, 303(8):739–746.
12. Jansen TC, van Bommel J, Schoonderbeek FJ, Sleeswijk Visser SJ, van der Klooster JM, Lima AP, Willemsen SP, Bakker J; LACTATE study group. Early lactate-guided therapy in intensive care unit patients: a multicenter, open-label, randomized controlled trial. Am J Respir Crit Care Med. 2010 Sep 15;182(6):752-61. doi: 10.1164/rccm.200912-1918OC. Epub 2010 May 12. [PubMed]
13. Weil MH, Afifi AA. Experimental and clinical studies on lactate and pyruvate as indicators of the severity of acute circulatory failure (shock). Circulation. 1970 Jun;41(6):989-1001. [PubMed]
14. Trzeciak S, Dellinger RP, Chansky ME, Arnold RC, Schorr C, Milcarek B, Hollenberg SM, Parrillo JE. Serum lactate as a predictor of mortality in patients with infection. Intensive Care Med. 2007 Jun;33(6):970-7. Epub 2007 Mar 13. [PubMed]
15. Helal NF, Samra NM, Abdel Ghany EAG et al: SNAP II in neonatal sepsis, J Neonatal boil;2013;2:121.
16. Jan Bakker, Maarten WN Nijsten and Tim C Jansen. Annals of Intensive Care 2013, 3:12 doi: 10.1186/2110-5820-3-12 Review.
Copyright (c) 2017 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


