Roux-en-Y hepaticojejunostomy versus hepaticoduodenostomy after excision of choledochal cyst: A randomized clinical trial and experience in a tertiary care hospital
Abstract
Introduction: Excision of choledochal cyst is required to relieve biliary obstruction thereby protecting the liver and pancreas as well as to prevent malignancy in long term. But controversy persists in the two existing techniques of biliary reconstruction after cyst excision.
Aim: To analyze the clinical presentation, incidence and types of choledochal cyst and our experience in management of these congenital anomalies. To compare the advantages and disadvantages between two modalities of biliary reconstruction.
Methods: A prospective, controlled, clinical trial was conducted on patients with choledochal cyst in a tertiary care pediatric surgery hospital. They were divided into two groups; Group–A: Patients in whom biliary reconstruction was done by Roux-en-Y hepaticojejunostomy, Group-B: Biliary reconstruction done by Hepaticoduodenostomy. The two groups were compared in respect to clinical course, types of cyst, surgical difficulties with special emphasis on operating time, postoperative complications.
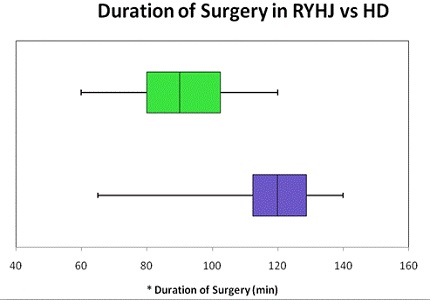
Results: Choledochal cysts accounted for 0.79% of total admissions at our institute. Out of 31 admitted cases, 22 cases were enrolled in the study. The number of patients in group A were 10 and in group B were 12. Abdominal pain was the commonest presenting feature and Type I choledochal cyst was the most common finding. The average duration of surgery was less in group B (1 hour 25 min) than in group A (2 hours and 10 min).
Conclusion: Biliary reconstruction by Hepaticoduodenostomy takes significantly less operative time than Roux-en-Y hepaticojejunostomy (P<0.05) and needs single anastomosis. It is more anatomical, physiological, easy to perform and associated with fewer complications.
Downloads
References
2. Thatipamula AB, Moka J. Surgical management of Choledochal cysts in children- Our experience in a district level teaching hospital. International Journal of Anatomy, Radiology and Surgery 2016; 5(4): SO05-08.
3. She WH, Chung HY, Lan LC, Wong KK, Saing H, Tam PK. Management of choledochal cyst: 30 years of experience and results in a single center. J Pediatr Surg. 2009 Dec;44(12):2307-11. doi: 10.1016/j.jpedsurg.2009.07.071.
4. Tadokoro H, Takase M. Recent advances in choledochal cysts. Open Journal of Gastroenterology 2012; 2: 145-154. http://dx.doi.org/10.4236/ojgas.2012.24029
5. Todani T, Watanabe Y, Narusue M, et al. Congenital bile duct cyst: Classification, operative procedure, and review of thirty-seven cases including cancer arising from choledochal cyst. Am J Surg 1977; 134(2): 263-9.
6. Lilly JR, Stellin GP, Karrer FM. Forme fruste choledochal cyst. J Pediatr Surg 1985;20(4): 449-51. [PubMed]
7. Liem NT, Holcomb III GW. Choledochal cyst and Gallbladder disease. In: Holcomb III GW, Murphy JP, Ostie DJ. Editors. Ashcraft’s Pediatric surgery. 6th ed. Elsevier Saunders 2014. Pp. 593-606.
8. Gonzales KD, Lee H. Choledochal Cyst. In: Coran AG, Adzick NS, Krummel TM, Laberge J, Shamberger RC, Caldmone AA. Editors. Pediatric Surgery. 7th ed. Elsevier Saunders 2012.pp. 1331-9.
9. Ono S, Fumino S, Shimadera S, Iwai N. Long-term outcomes after hepaticojejunostomy for choledochal cyst: a 10- to 27-year follow-up. J Pediatr Surg. 2010 Feb;45(2):376-8. doi: 10.1016/j.jpedsurg.2009.10.078. [PubMed]
10. Shimotakahara A, Yamataka A, Yanai T, Kobayashi H, Okazaki T, Lane GJ, Miyano T. Roux-en-Y hepaticojejunostomy or hepaticoduodenostomy for biliary reconstruction during the surgical treatment of choledochal cyst: which is better? Pediatr Surg Int. 2005 Jan;21(1):5-7.
11. Sharma A, Pandey A, Rawat J, Ahmed I, Wakhlu A. Conventional and unconventional surgical modalities for choledochal cyst: Long-term follow-up. Annals of Pediatric Surgery 2011; 7(1): 17-9.
12. Bhavsar MS, Vora HB, Giriyappa VH. Choledochal cysts : a review of literature. Saudi J Gastroenterol. 2012 Jul-Aug;18(4):230-6. doi: 10.4103/1319-3767.98425. [PubMed]
13. Howard ER, Choledochal cysts. In: Howard ER. Editor. Surgery of liver disease in children. Butterworth-Heineman, Oxford 1991. Pp. 78-90.
14. Lipsett PA, Pitt HA. Surgical treatment of choledochal cysts. J Hepatobiliary Pancreat Surg. 2003;10(5):352-9. [PubMed]
15. Liu BS, Shu YP, Xing KM, Cheng HP, Ying BL, Xiao PC. Diagnosis and treatment of congenital choledochal cyst: 20 years’ experience in China. World J Gastroenterol 2001; 7: 733-4.
16. Miyano T, Yamataka A, Li L. Congenital biliary dilatation. Semin Pediatr Surg. 2000 Nov;9(4):187-95. [PubMed]
17. Babbitt DP. [Congenital choledochal cysts: new etiological concept based on anomalous relationships of the common bile duct and pancreatic bulb]. Ann Radiol (Paris). 1969;12(3):231-40.
18. Jabłońska B. Biliary cysts: etiology, diagnosis and management. World J Gastroenterol. 2012 Sep 21;18(35):4801-10. [PubMed]
19. Singham J, Yoshida EM, Scudamore CH. Choledochal cysts: part 1 of 3: classification and pathogenesis. Can J Surg. 2009 Oct;52(5):434-40. [PubMed]
20. Davenport M, Basu R. Under pressure: choledochal malformation manometry. J Pediatr Surg. 2005 Feb;40(2):331-5. [PubMed]
21. Komi N, Takehara H, Kunitomo K, Miyoshi Y, Yagi T. Does the type of anomalous arrangement of pancreaticobiliary ducts influence the surgery and prognosis of choledochal cyst? J Pediatr Surg. 1992;27:728–31. DOI: http://dx.doi.org/10.1016/S0022-3468(05)80102-2. [PubMed]
22. Mukhopadhyay B, Shukla RM, Mukhopadhyay M, Mandal KC, Mukherjee PP, Roy D, Biswas SK, Basu KS. Choledochal cyst: A review of 79 cases and the role of hepaticodochoduodenostomy. J Indian Assoc Pediatr Surg. 2011 Apr;16(2):54-7. doi: 10.4103/0971-9261.78131.
23. Lipsett PA, Pitt HA, Colombani PM, Boitnott JK, Cameron JL. Choledochal cyst disease. A changing pattern of presentation. Ann Surg. 1994 Nov;220(5):644-52. [PubMed]
24. Metcalfe MS, Wemyss-Holden SA, Maddern GJ. Management dilemmas with choledochal cysts. Arch Surg. 2003 Mar;138(3):333-9.
25. Chijiiwa K, Koga A. Surgical management and long-term follow-up of patients with choledochal cysts. Am J Surg. 1993 Feb;165(2):238-42. [PubMed]
26. Watanabe Y, Toki A, Todani T. Bile duct cancer developed after cyst excision for choledochal cyst. J Hepatobiliary Pancreat Surg. 1999;6(3):207-12.
27. Lilly JR. The surgical treatment of choledochal cyst. Surg Gynecol Obstet. 1979 Jul;149(1):36-42. [PubMed]
28. Hata Y, Sasaki F, Takahashi H, Tamura M, Ohkawa Y, Saji Y, Kurauchi N, Manabe K, Uchino J. Surgical treatment of congenital biliary dilatation associated with pancreaticobiliary maljunction. Surg Gynecol Obstet. 1993 Jun;176(6):581-7.
29. Yamataka A, Ohshiro K, Okada Y, et al. Complications after cyst excision with hepaticoenterostomy for choledochal cysts and their surgical management in children versus adults. J Pediatr Surg 1997; 32: 1097-1102.Doi:10.1016/S0022-3468(97)90407-3.
30. Narayanan SK, Chen Y, Narasimhan KL, Cohen RC. Hepaticoduodenostomy versus hepaticojejunostomy after resection of choledochal cyst: a systematic review and meta-analysis. J Pediatr Surg. 2013 Nov;48(11):2336-42. doi: 10.1016/j.jpedsurg.2013.07.020.
31. Todani T, Watanabe Y, Mizuguchi T, Fujii T, Toki A. Hepaticoduodenostomy at the hepatic hilum after excision of choledochal cyst. Am J Surg. 1981 Nov;142(5):584-7. [PubMed]
Copyright (c) 2017 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


