Factors Affecting Peak Expiratory Flow Rates in Children of 9–12 Years of Age
Abstract
Introduction: Documentation of peak expiratory flow rate (PEFR) variability may be used to support the diagnosis of asthma and other respiratory disorders.
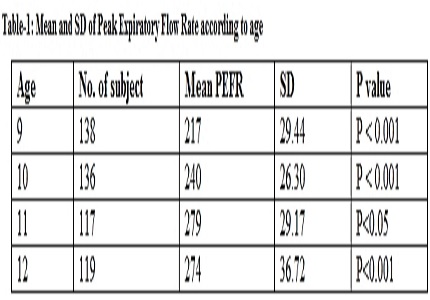
Methodology: This study was carried to measure PEFR of 510 children age group 9 to 12 years of both sexes using a Mini WrightTM Peak Flow Meter. Results were analyzed to find out the normal values of peak expiratory flow rate at each age and either sex. The results were also analyzed to find out what factors influence the peak expiratory flow rate. Effect of age, sex, height, weight, chest circumference, socioeconomic status, passive smoking, cooking fuel, history of contact with tuberculosis and bronchial asthma in family were analyzed separately.
Results: The average peak expiratory flow rate in boys was 272±53.16 L/min and for girls was 252±45.09 L/min. For the given age boys have higher peak expiratory flow rate than girls. The peak expiratory flow rate shows very good correlation with height and weight in both sexes. A History of contact with tuberculosis is associated with lower peak expiratory flow rate. Children coming from homes with firewood being used as a fuel and passive smoking had lower peak expiratory flow-rate. No significant relation has been found between peak expiratory flow rate and socioeconomic status and family history of bronchial asthma.
Conclusions:The peak expiratory flow rate values of children in study region were comparatively low to those of North Indian and Western children but more compared to urban south Indian children.
Downloads
References
2. Raju PS, Prasad KV, Ramana YV, Murthy KJ.Pulmonary function tests in Indian girls--prediction equations.Indian J Pediatr.2004Oct;71(10):893-7. [PubMed]
3. Spruit MA, Singh SJ, Garvey C, et al ATS/ERS Task Force on PulmonaryRehabilitation. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation.Am J RespirCrit Care Med.2013Oct15;188(8):e13-64. doi: 10.1164/rccm.201309-1634ST. [PubMed]
4. Gøtzsche PC, Johansen HK. House dust mite control measures for asthma: systematic review.Allergy. 2008 Jun;63(6):646-59. doi: 10.1111/j.1398-9995.2008.01690.x. [PubMed]
5. van der Kooi E, Klarenbeek NB, Güler-Yüksel M, Kerstens PJ, van der Lubbe PA, Westedt ML, ten Wolde S, Huizinga TW, Dijkmans BA, Allaart CF. A decrease in disease activity score (DAS) level is associated with a decrease in health assessment questionnaire (HAQ) score, independent of follow-up duration, during 5 years of tightly controlled treatment: results from the BeSt study.Ann Rheum Dis. 2011 Jan;70(1):168-71. doi: 10.1136/ard.2010.133132. Epub 2010 Nov 29. [PubMed]
6. Sharma R. Kuppuswamy's socioeconomic status scale--revision for 2011 and formula for real-time updating.Indian J Pediatr. 2012 Jul;79(7):961-2. doi: 10.1007/s12098-011-0679-3. Epub 2012 Jan 10.
7. Donaldson GC, Seemungal TA, Bhowmik A, Wedzicha JA.Relationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary disease.Thorax.2002Oct;57(10):847-52. [PubMed]
8. Janssens JP, Pache JC, Nicod LP.Physiological changes in respiratory function associated with ageing.EurRespir J.1999Jan;13(1):197-205. [PubMed]
9. Steffen TM, Hacker TA, Mollinger L. Age- and gender-related test performance in community-dwelling elderly people: Six-Minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and gait speeds.Phys Ther.2002Feb;82(2):128-37. [PubMed]
10. Peterson ML, Jacobs DR Jr, Milla CE.Longitudinal changes in growth parameters are correlated with changes in pulmonary function in children with cystic fibrosis.Pediatrics.2003Sep;112(3 Pt 1):588-92.
11. Singh AK, Cydulka RK, Stahmer SA, Woodruff PG, Camargo CA. Sex differences among adults presenting to the emergency department with acute asthma. Archives of internal medicine. 1999 Jun 14;159(11):1237-43.
12. Mohammadzadeh I, Gharagozlou M, Fatemi SA. Normal values of peak expiratory flow rate in children from the town of Babol, Iran.Iran J Allergy Asthma Immunol. 2006 Dec;5(4):195-8.
13. Eigen H, Bieler H, Grant D, Christoph K, Terrill D, Heilman DK, Ambrosius WT, Tepper RS.Spirometric pulmonary function in healthy preschool children.Am J RespirCrit Care Med.2001Mar;163(3 Pt 1):619-23. [PubMed]
14. Pulickal AS, Fernandez GV. Peak expiratory flow rate in healthy rural south Indian school children predicted from body height. Editorial Board Vol. 51 No. 2 April-June 2007. 2007 Apr 5;51(2).
15. Jackson B, Kubzansky LD, Cohen S, Weiss S, Wright RJ. A matter of life and breath: childhood socioeconomic status is related to young adult pulmonary function in the CARDIA study. International journal of epidemiology. 2004 Apr 1;33(2):271-8.
16. Kosmidis C, Denning DW. The clinical spectrum of pulmonary aspergillosis.Thorax.2015 Mar;70(3):270-7. doi: 10.1136/thoraxjnl-2014-206291. Epub 2014 Oct 29. [PubMed]
17. Palmer CN, Doney AS, Lee SP, Murrie I, Ismail T, Macgregor DF, Mukhopadhyay S. Glutathione S-transferase M1 and P1 genotype, passive smoking, and peak expiratory flow in asthma.Pediatrics. 2006 Aug;118(2):710-6.
18. Li YF, Gilliland FD, Berhane K, Mcconnell RO, James Gauderman W, Rappaport EB, Peters JM. Effects of in utero and environmental tobacco smoke exposure on lung function in boys and girls with and without asthma. American journal of respiratory and critical care medicine. 2000 Dec 1;162(6):2097-104.
19. Tsai CH, Huang JH, Hwang BF, Lee YL. Household environmental tobacco smoke and risks of asthma, wheeze and bronchitic symptoms among children in Taiwan. Respiratory research. 2010 Dec 1;11(1):11.
20. Chhabra SK, Chhabra P, Rajpal S, Gupta RK.Ambient air pollution and chronic respiratory morbidity in Delhi.Arch Environ Health.2001Jan-Feb;56(1):58-64. [PubMed]
21. Urom SE, Antai AB, Osim EE. Symptoms and lung function values in Nigerian men and women exposed to dust generated from crushing of granite rocks in Calabar, Nigeria. Nigerian Journal of Physiological Sciences. 2004;19(1):41-7.
22. Smith AD, Cowan JO, Filsell S, McLachlan C, Monti-Sheehan G, Jackson P, Taylor DR.Diagnosing asthma: comparisons between exhaled nitric oxide measurements and conventional tests.Am J RespirCrit Care Med.2004Feb15;169(4):473-8. Epub 2003 Nov 25. [PubMed]
23. Pellegrino R, Viegi G, Brusasco V, Crapo RO, Burgos F, Casaburi R, Coates A, van der Grinten CP, Gustafsson P, Hankinson J, Jensen R, Johnson DC, MacIntyre N, McKay R, Miller MR, Navajas D, Pedersen OF, Wanger J.Interpretative strategies for lung function tests.EurRespir J.2005Nov;26(5):948-68. [PubMed]
Copyright (c) 2017 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


