Antibiotics prescription pattern and compliance for common childhood illnesses – an observational study
Abstract
Introduction: Antibiotics are generally overused in children. Frequent inappropriate use of antibiotics and poor compliance contributes to antibiotic resistance. An observational study was undertaken to determine the pattern of antibiotic use and compliance for common ailments in children attending a tertiary care hospital in Puducherry, South India.
Methods: Data was obtained from 197 consecutive children who had visited a health care provider during the previous two weeks for any ailment, in a pretested semi structured questionnaire. Data was entered on MS Excel spreadsheet and analysed using Stata14.0 (Stata Corp, College Station, Tx). Chi square test with Fisher’s modification and logistic regression models were used in the analysis.
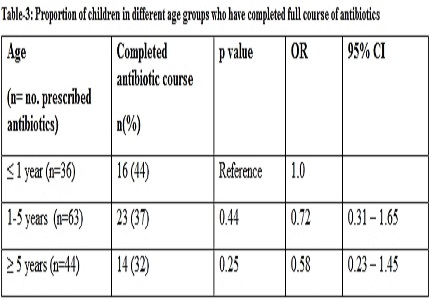
Results: Acute respiratory infections were the most common infections in all age groups followed by diarrheal disorders in infants and fever in older children. Proportion of illnesses which received antibiotics was 75% for respiratory illnesses, 78% for fever, 50% for diarrheal disorders and 64% for other infections, there being no statistically significant difference between them. Out of 143 children who were prescribed antibiotics, 127 (89%) gave the medicines as prescribed. However, only 53 (37%) completed the full course of antibiotics. Compliance with treatment was not associated with age or the type of illness. Most of the parents (73%) discontinued antibiotics because of worsening of symptoms. Adverse reaction to antibiotics was seen in 32 (22%) children.
Conclusion: Overuse of antibiotics for common ailments and poor compliance with treatment were perhaps important contributory causes for development of antimicrobial resistance in this region.
Downloads
References
2. Batwala V, Magnussen P, Nuwaha F. Antibiotic use among patients with febrile illness in a low malaria endemicity setting in Uganda. Malar J. 2011 Dec 20;10:377. doi: 10.1186/1475-2875-10-377. [PubMed]
3. Abbas S, Ihle P, Heymans L, Kupper-Nybelen J, Schubert I.Differences in antibiotic prescribing between general practitioners and pediatricians in Hesse, Germany. Dtsch Med Wochenschr.2010 Sept;135 (37):1792-97. doi: 10.1055/s-0030-1263321.
4. Chandy SJ, Thomas K, Mathai E, Antonisamy B, Holloway KA, Stalsby Lundborg C. Patterns of antibiotic use in the community and challenges of antibiotic surveillance in a lower-middle-income country setting: a repeated cross-sectional study in Vellore, South India. J Antimicrob Chemother. 2013 Jan;68(1):229-36. doi: 10.1093/jac/dks355. Epub 2012 Sep 3. [PubMed]
5. Pathak A, Mahadik K, Dhaneria SP, Sharma A, Eriksson B, Lundborg CS. Antibiotic prescribing in outpatients: Hospital and seasonal variations in Ujjain, India. Scand J Infect Dis. 2011 Jul;43(6-7):479-88. doi: 10.3109/00365548.2011.554854. Epub 2011 Feb 7.
6. Bapna JS, Tekur U, Gitanjali B, Shashindran CH, Pradhan SC, Thulasimani M, Tomson G. Drug utilization at primary health care level in southern India. Eur J Clin Pharmacol. 1992;43(4):413-5. [PubMed]
7. Kumar R, Indira K, Rizvi A, Rizvi T, Jeyaseelan L. Antibiotic prescribing practices in primary and secondary health care facilities in Uttar Pradesh, India. J Clin Pharm Ther. 2008 Dec;33(6):625-34. doi: 10.1111/j.1365-2710.2008.00960.x. [PubMed]
8. Hadi U, Duerink DO, Lestari ES, Nagelkerke NJ, Keuter M, Huis In't Veld D, Suwandojo E, Rahardjo E, van den Broek P, Gyssens IC; Antimicrobial Resistance in Indonesia: Prevalence and Prevention. Audit of antibiotic prescribing in two governmental teaching hospitals in Indonesia. Clin Microbiol Infect. 2008 Jul;14(7):698-707. doi: 10.1111/j.1469-0691.2008.02014.x. [PubMed]
9. Casey JR, Marsocci SM, Murphy ML, Francis AB, Pichichero ME. White blood cell count can aid judicious antibiotic prescribing in acute upper respiratory infections in children. Clin Pediatr (Phila). 2003 Mar;42(2):113-9. [PubMed]
10. Vodicka TA, Thompson M, Lucas P, Heneghan C, Blair PS, Buckley DI, Redmond N, Hay AD; TARGET Programme team. Reducing antibiotic prescribing for children with respiratory tract infections in primary care: a systematic review. Br J Gen Pract. 2013 Jul;63(612):e445-54. doi: 10.3399/bjgp13X669167. [PubMed]
11. Cantón R, Bryan J. Global antimicrobial resistance: from surveillance to stewardship. Part 2: stewardship initiatives. Expert Rev Anti Infect Ther. 2012 Dec;10(12):1375-7. doi: 10.1586/eri.12.140. [PubMed]
12. Bozic B, Bajcetic M. Use of antibiotics in paediatric primary care settings in Serbia. Arch Dis Child. 2015 Oct;100(10):966-9. doi: 10.1136/archdischild-2015-308274. Epub 2015 May 20. [PubMed]
13. De Luca M, Dona D, Montagnani C, Lo Vecchio A,Romanengo M,Tagliabue C, et al. Antibiotic Prescriptions and Prophylaxis in Italian Children. Is It Time to Change? ARPEC Project PLoS One.2016;11: e0154662. https://doi.org/10.1371/journal.pone.0154662.
14. Borras Novell C, Hernandez Bou S, Garcia Garcia J J. Prescribing of antibiotics in patients admitted from Emergency Departments:a multicenter study.An Pediatr (Barc).2013July;79(1):15-20. doi: 10.1016 /j.anpedi.2012.09.003.
15. Sharma M, Damlin A, Pathak A, Lundborg S C. Antibiotic Prescribing among Pediatric Inpatients with Potential Infections in Two Private Sector Hospitals in Central India. PLoS One; 2015;10: e0142317. https://doi.org/10.1371/journal.pone.0142317.
16. Siddiqi S, Hamid S, Rafique G, Chaudhry SA, Ali N, Shahab S, Sauerborn R. Prescription practices of public and private health care providers in Attock District of Pakistan. Int J Health Plann Manage. 2002 Jan-Mar;17(1):23-40. [PubMed]
17. Holstiege J, Garbe E. Systemic antibiotic use among children and adolescents in Germany: a population-based study. Eur J Pediatr. 2013 Jun;172(6):787-95. doi: 10.1007/s00431-013-1958-y. Epub 2013 Feb 10.
18. Koura K G, Garcia A, Todoegnon B, Deloron P, Cot M, Faucher J F. Prevalence and factors related to antibiotic prescription in Benin: a school-based study. Acta Trop.2013 Aug;127(2):87-90. doi: 10.1016/j.actatropica.2013.04.004.
19. Nizami SQ, Khan IA, Bhutta ZA. Paediatric prescribing in Karachi. J Pak Med Assoc. 1997 Jan;47(1):29-32.
20. Bharathiraja R, Sridharan S, Chelliah LR, Suresh S, Senguttuvan M. Factors affecting antibiotic prescribing pattern in pediatric practice. Indian J Pediatr. 2005 Oct;72(10):877-9. [PubMed]
21. Angoulvant F, Skurnik D, Bellanger H, Abdoul H, Bellettre X, Morin L, et al. Impact of implementing French antibiotic guidelines for acute respiratory-tract infections in a paediatric emergency department, 2005-2009. Eur J Clin Microbiol Infect Dis. 2012 July; 31(7): 1295-1303. doi=10.1007/s10096-011-1442-4.
22. De Brasi D, Pannuti F, Antonelli F, de Seta F, Siani P, de Seta L. Therapeutic approach to bronchiolitis: why pediatricians continue to overprescribe drugs? Ital J Pediatr. 2010 Oct 1;36:67. doi: 10.1186/1824-7288-36-67.
23. Osatakul S, Puetpaiboon A. Appropriate use of empirical antibiotics in acute diarrhoea: a cross-sectional survey in southern Thailand. Ann Trop Paediatr. 2007 Jun;27(2):115-22.
24. Pathak D, Pathak A, Marrone G, Diwan V, Lundborg CS. Adherence to treatment guidelines for acute diarrhoea in children up to 12 years in Ujjain, India--a cross-sectional prescription analysis. BMC Infect Dis. 2011 Jan 28;11:32. doi: 10.1186/1471-2334-11-32.
25. Biswas M, Roy D N, Tajmim A, Rajib S S, Hossain M, Farzana F, Yasmen N.Prescription antibiotics for outpatients in Bangladesh: a cross-sectional health survey conducted in three cities. Ann Clin Microbiol Antimicrob.2014 Apr;13: 15. https://doi.org/10.1186/1476-0711-13-15.
Copyright (c) 2017 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


