A study on growth profiles in children with thalassemia major between 2-10 years of age on regular transfusions and oral chelation therapy
Abstract
Introduction: Thalassemia patients require regular blood transfusions to maintain haemoglobin level around 10gm/dl, which results in transfusional iron over load which is treated by well-established parenteral desferrioxamine or oral chelators. There are conflicting reports on effectiveness of oral chelators. Only few studies are available on the growth parameters of thalassemic children from this region. The present study was under taken to assess the growth pattern and its relation with Mean Pre-transfusion Haemoglobin value and Serum ferritin concentration in study population.
Materials and Methods: The present study was done at Thalassemia and Sickle CellSociety, Hyderabad. The study group includes Transfusion dependent thalassemia major children on oral Iron Chelation Therapy between 2-10 years of age. Specific inclusion and exclusion criteria were framed and subjects fulfilling the criteria were selected for the study. Anthropometry of the children was measured and necessary data from the medical records of the children was reviewed during the study period September 2012 to May 2013.
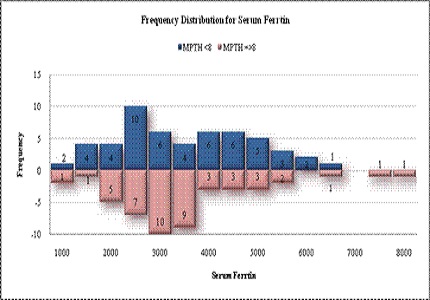
Results: In Mean pre transfusion haemoglobin <8 g/dl group, all the children are below median weight for age and Height for age Z scores whereas in Mean pre transfusion haemoglobin ≥8g/dl,group, 12.3% of the children are above the median Weight for age Z score and 6.2% of the children above the median Height for age Z score. Weight for age or Height for age Z scores has no correlation with age.With the increasing age, more thalassemic children had growth retardation, Height being affected more than Weight.
Conclusion: Growth of thalassemic children during the first decade largely depends upon the maintenance of fairly normal haemoglobin between 9.5-10gm% with frequent blood transfusions and adequate chelation.
Downloads
References
2. Quirolo Keith and Elliot Vichinsky. Thalassemia syndromes. In: Nelson Text book of Pediatrics, 19th edn. Behrman RE, Kliegman RM and Jenson HB (eds). India. Elsevier, 2012, 1674-78.
3. Weatherall DJ. The thalassemias. In: Stamatoyannopoulos G, Nienhuis AW, Majerus PH, Varmus H, eds. The molecular basis of blood diseases. 2nd ed. Philadelphia: W.B. Saunders, 1994:157-205.
4. Weatherall DJ. Common genetic disorders of the red cell and the "malaria hypothesis" Annals of Tropical Medicine Parasitology 1987; 81:539-548.
5. Choudhry V.P, R.Kashyap, S.K. Acharya, N. Tandon, A. Saxena. Challenges in the Management of Thalassaemia, Mediquest Medical Information series - 1997: Vol. 15 : No.3: 1-9.
6. Gorstein J, Sullivan KM, Parvanta I, Begin F. Indicators and methods for cross-sectional surveys of vitamin and mineral status of populations. Micronutrient Initiative (Ottawa) and Centers for Disease Control and Prevention (Atlanta), May 2007, pg 29).
7. Thacker N. Prevention of thalassemia in India.Indian Pediatr. 2007 Sep;44(9):647-8. [PubMed]
8. Sharma R. Kuppuswamy's socioeconomic status scale--revision for 2011 and formula for real-time updating.Indian J Pediatr. 2012 Jul;79(7):961-2. doi: 10.1007/s12098-011-0679-3. Epub 2012 Jan 10.
9. WHO anthrosoftware(www.who.int/childgrowth/software/
10. http://www.who.int/childgrowth/standards
11. Pemde, Harish, Chandra Jagdish, Gupta Divya, Singh Varinder, Sharma, Rajni, Dutta, Ak. Physical growth in children with transfusion-dependent thalassemia. Pediatric Health, Medicine and Therapeutics. 2011. 2-13. 10.2147/PHMT.S15305.
12. Tienboon P, Sanguansermsri T, Fuchs GJ. Malnutrition and growth abnormalities in children with beta thalassemia major. Southeast Asian J Trop Med Public Health. 1996 Jun;27(2):356-61.
13. Singhal B, Shama N and Mathur R. Iron Overload and Growth of Thalassemic Patients in Marwar Region. Int J Pharm Sci Res, 2012; Vol. 3(7): 2043-2049.
14. Trehan P, Madan N, Ghai OP, Sood SK. Beta-thalassaemia syndromes as seen in Northern India.Indian Pediatr. 1980 Mar;17(3):219-26.
15. Reddy YR et al. Brief communication, thalassemia in Andhra Pradesh- a clinicohaematological study. Indian paediatrics 1975; 12:195-199.
16. George A, Bhaduri A, Sen S, Choudhry VP. Physical growth parameters in thalassemic children.Indian J Pediatr. 1997 Nov-Dec;64(6):861-71.
17. Sunil Gomber, Rohit Saxena, Nishi Madan. Comparative efficacy of Desferrioxamine, Deferiprone and in combination on Iron Chelation in Thalassemic Children. Indian paediatrics2004;41:21-26.
18. Olivieri NF, et al. Long-Term Safety and Effectiveness of Iron Chelation Therapy with Deferiprone for Thalassemia Major. New England journal of Medicine.1998; 339:417-423.
Copyright (c) 2018 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


