Study of neuro developmental outcome of hypoxic ischemic encephalopathy of less than one-year infant in a tertiary care institute
Abstract
Introduction: Perinatal asphyxia can lead to hypoxic ischemic encephalopathy (HIE). The mortality due to hypoxic ischemic encephalopathy is as high as 28.8 % and morbidity is 30 % of surviving new-born due to hypoxic ischemic encephalopathy.
Aim & Objective: To study the neuro developmental outcome of surviving neonate with hypoxic ischemic encephalopathy till one year of age and to give early stimulation to such baby to decrease the morbidity.
Material & Method: It isa hospital based prospective study done in tertiary care hospital in SCB Medical College Hospital & SVP PG Institute, Cuttack from July 2015 to June 2017.
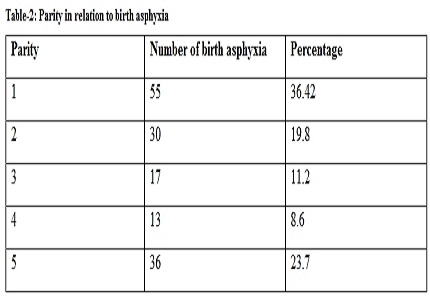
Result: The incidence of asphyxia neonatorum among the babies in normal delivery was very high compared to the babies of lower section caesarean section (LSCS) delivery. Severity of birth asphyxia was high in face presentation, followed by breech than normal vertex presentation. Respiratory distress was found to be associated with neonatal asphyxia in this study. Mortality is highest in severe encephalopathy and least in mild variety. In follow, up study neurodevelopmental abnormality is found to be 100% in HIE-III. 34.4% in HIE-II and normal development in stage –I HIE.
Conclusion: Institutional delivery with trained personal with neonatal resuscitation at first golden minute will prevent birth asphyxia. Timely screening of asphyxiated babies and early sensory stimulation decreases the morbidity in asphyxiated newborn.
Downloads
References
2. Fisher DL, Fraser BJ. School climate: assessing and Improving School Environments,Set,(1990). 4,2.
3. McIntosh N. The Newborn. In: McIntosh N, Helms PJ, Smyth LR, editors. Forfar&Arneil’s Textbook of Pediatrics. 7th ed. New York: Churchill Livingstone 2008:177-392.
4. Agarwal R, Jain A, Deorari AK, Paul VK. Post-resuscitation management of asphyxiated neonates. Indian J Pediatr. 2008 Feb;75(2):175-80. [PubMed]
5. M J Sankar, S B Neogi, J Sharma,MChauhan,R Srivastava, P K Prabhakar, A Khera,R Kumar, S Zodpey and V K Paul.State of newborn health in India. J Perinatol 2016 Dec; 36(Suppl 3): S3–S8. [PubMed]
6. Kimberly A. Allen, Debra H. Brandon, Hypoxic Ischemic Encephalopathy: Pathophysiology and Experimental Treatments Newborn Infant Nurs Rev. 2011 Sep 1; 11(3): 125–133.
7. Anne CC Lee,Luke C. Mullany, James M. Tielsch, Joanne Katz, Subarna K. Khatry, Steven C. LeClerq, Ramesh K. Adhikari,Shardaram R. Shrestha, and Gary L. Darmstadt, Risk Factors for Neonatal Mortality due to Birth Asphyxia in Southern Nepal;Pediatrics. 2008 May; 121(5): e1381–e1390.
8. Reshma Parvin Sampa, QuaziZahangir Hossain and Sabia Sultana. Observation of Birth Asphyxia and Its Impact on Neonatal Mortality in Khulna Urban Slum Bangladesh. International Journal of Advanced Nutritional and Health Science 2012: 1,( 1);1-8, Article ID Med-27.
9. Sarnat HB, Sarnat MS. Neonatal encephalopathy following fetal distress. A clinical and electroencephalographic study. Arch Neurol. 1976 Oct;33(10):696-705.
10. Sharma V, Katz J, Mullany LC, Khatry SK, LeClerq SC, Shrestha SR, Darmstadt GL, Tielsch JM. Young maternal age and the risk of neonatal mortality in rural Nepal. Arch PediatrAdolesc Med. 2008 Sep;162(9):828-35. doi: 10.1001/archpedi.162.9.828.
11. Lee AC, Mullany LC, Tielsch JM, Katz J, Khatry SK, LeClerq SC, Adhikari RK, Shrestha SR, Darmstadt GL. Risk factorsforneonatal mortalityduetobirth asphyxiainsouthernNepal: aprospective, community-basedcohort study. Pediatrics.2008May;121(5):e1381-90. doi: 10.1542/peds.2007-1966.
12. Ilan Arad. Does parity affect the neonatal outcome of very-low-birth-weight infants ?European journal of obstretrics, Gynaecology and Reproductive Biology2001;94(2):pg283-288
13. Kapur S, Mammen KG, Mathew KC, Kumar G. Asphyxia neonatorum. Indian Pediatr. 1970 May;7(5):276-80.
14. Dweck HS, Huggins W, Dorman LP, Saxon SA, Benton JW, Jr, Cassady G. Developmental sequelae in infants having suffered severe perinatal asphyxia. Am J Obstet Gynecol. 1974 Jul 15;119(6):811-5.
15. Chandra S, Ranji S, ThirupuramS.. Perinatal asphyxia multivariate analysis of risk factor in hospital births. Indian Pediatr 1997; 34 : 206- 212.
16. Chaturvedi P, Shah N. Foetal co-relates and mode of delivery in asphyxia neonatorum. Indian J Pediatr. 1991 Jan-Feb;58(1):63-7. [PubMed]
17. Batra A, Sen Gupta A, Kumar A. A study of asphyxia neonatorum. J Obs& Gynae India, 1988; 162-166.
18. Bhandari N, Bahl R, Taneja S, Martines J, Bhan MK. Pathways to infant mortality in urban slums of Delhi, India: implications for improving the quality of community- and hospital-based programmes. J Health PopulNutr. 2002 Jun;20(2):148-55.
19. Perlman JM1, Tack ED, Martin T, Shackelford G, Amon E. Acute systemic organ injury in term infants after asphyxia. Am J Dis Child. 1989 May;143(5):617-20.
20. Martín-Ancel A, García-Alix A, Gayá F, Cabañas F, Burgueros M, Quero J. Multipleorganinvolvement in perinatalasphyxia. J Pediatr.1995 Nov;127(5):786-93.
21. Elder DE, Zuccollo JM, Stanley TV. Neonatal deathafterhypoxic ischaemic encephalopathy: does a postmortemadd to the finaldiagnoses? BJOG.2005 Jul;112(7):935-40. [PubMed]
22. Levene MI, Sands C, Grindulis H, Moore JR. Comparison of twomethods of predictingoutcome in perinatalasphyxia. Lancet.1986Jan11;1(8472):67-9. [PubMed]
23. Charlene MT Robertson, Max Perlman. Follow-up of the term infant after hypoxic-ischemic encephalopathy Paediatr Child Health. 2006 May; 11(5): 278–282.
24. Dixon G, Badawi N, Kurinczuk JJ, Keogh JM, Silburn SR, Zubrick SR, Stanley FJ. Earlydevelopmentaloutcomesafternewbornencephalopathy. Pediatrics. 2002 Jan;109(1):26-33. [PubMed]
25. Carli G1, Reiger I, Evans N. One-year neurodevelopmental outcome after moderate newborn hypoxic ischaemic encephalopathy. J Paediatr Child Health. 2004 Apr;40(4):217-20.
26. Seetha Shankaran, Abbot R. Laptook, Jon E. Tyson, Scott A. Mc Donald , Edward F. Donovan et al , Whole-Body Hypothermia for Neonates with Hypoxic–Ischemic Encephalopathy N Engl J Med 2005; 353:1574-1584.
27. Marlow N, Rose AS, Rands CE, Draper ES. Neuropsychological and educational problems at school age associated with neonatal encephalopathy Arch Dis Child Fetal Neonatal Ed. 2005 Sep;90(5):F380-7.
Copyright (c) 2018 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


