A study of Neonatal Sepsis and to assess the validity of sepsis screen as a diagnostic tool
Abstract
Introduction: Neonatal sepsis is the leading cause of neonatal mortality in the developing world. There is an increasing incidence of drug resistance among organisms. We have tried to the sepsis profile in our nursery and to assess the validity of sepsis screen as a diagnostic tool. We have also studied the individual parameters of the screen for their strength as a diagnostic tool.
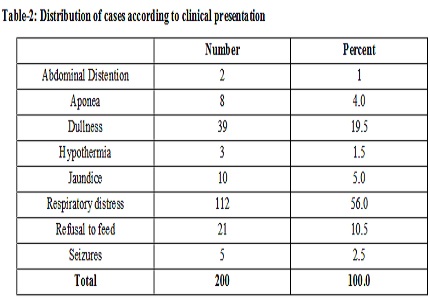
Methods: This was a prospective study carried out in the SCNU of MY Hospital and included 200 newborns with suspected sepsis. Sepsis Screen and Blood Cultures were done in all the babies and the results were analysed.
Results: Out of the 200 patients with suspected sepsis, 150 (75%) had a positive sepsis screen whereas 102 (51%) were culture positive. Sepsis Screen was positive in 93.1% of total culture positive sepsis and in 56.1% of culture negative cases too. Thus, the Sensitivity and specificity for Septic Screen was calculated to be 93.18 and 43.88% repetitively. PPV was 63.33% and NPV was 86.0 %.
Conclusion: The bacteriological flora has changed over the last 12 years and there has been a high incidence of resistance to the first live antibiotics in our Nursery. The sepsis screen has a high negative predictive value and it is recommended that negative sepsis screen should warrant discontinuation of the empirical antibiotics to prevent the unnecessary use and the emergence of drug resistant organisms.
Downloads
References
2. Liu L, Johnson HL, Cousens S, et al. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet 2012; 379:2151–61.
3. Thaver D, Zaidi AKM. Burden of neonatal infections in developing countries: a review of evidence from community based studies. Pediatr Infect Dis J 2009;28(1 Suppl): S3–9.
4. Gerdes JS, Polin R. Early diagnosis and treatment of neonatal sepsis. Indian J Pediatr; Jan-Feb 65(1):63-78. [PubMed]
5. Da Silva O, Ohlsson A, Kenyon C. Accuracy of leukocyte indices and C-reactive protein for diagnosis of neonatal sepsis: a critical review. Pediatr Infect Dis J 1995; 14:362-6
6. WHO Handbook IMCI Integrated Management of Childhood Illnesses. WHO/FCH/CAH/00. 12 Geneva: WHO 2000.
7. Weber MW, Carlin JB, Gatchalian S, Lehmann D, Muhe L, Mulholland EK, et al. Predictors of neonatal sepsis in developing countries. Pediatrics Infect Dis J2003; 22(8):711-7.
8. Shah AJ, Mulla SA, Revdiwala SB. Neonatal sepsis: High antibiotic resistance of the bacterial pathogens in a neonatal intensive care unit of a tertiary care hospital. J Clin Neonatol. 2012; 1:72–5. [PMC free article]
9. Shaw CK, Shaw P, Thapalial A. Neonatal sepsis bacterial isolates and antibiotic susceptibility patterns at a NICU in a tertiary care hospital in western Nepal: a retrospective analysis. KUMJ. 2007; 5:153–60. [PubMed].
10. Bhattacharjee A, Sen MR, Prakash P, Gaur A, Anuprabha S. Increased prevalence of extended spectrum β – Lactamase producers in neonatal septicemic cases at tertiary referral hospital. Indian J Med Microbiol. 2008; 26:356–60.
11. Buttery JP. Blood cultures in newborn and children: optimizing an everyday test. Arch Dis Child Fetal Neonatal Ed. 2002;87: F25–7. [PubMed]
12. Rajaratnam JK, Marcus JR, Flaxman AD, Wang H, Levin-Rector A, Dwyer L, et al. Neonatal, post-neonatal, childhood, and under-5 mortality for 187 countries, 1970-2010: a systematic analysis of progress towards Millennium Development Goal 4. Lancet. 2010; 375:1988-2008.
13. Sharma CM, Agrawal RP, Sharan H, Kumar B, Sharma D, Bhatia SS. Neonatal Sepsis": Bacteria & amp; their Susceptibility Pattern towards Antibiotics in Neonatal Intensive Care Unit. J Clin Diagn Res. 2013 Nov;7 (11):2511-3.
14. Vesikari T, Janas M, Gronroos P, 'Tuppurainen N, Renlund M, Kero P, et al. Neonatal septicemia. Arch Dis Child 1985; 60: 542-546.
15. Thakur S, Thakur K, Sood A, Chaudhary S. Bacteriological profile and antibiotic sensitivity pattern of neonatal septicaemia in a rural tertiary care hospital in North India. Indian J Med Microbiol 2016; 34:67-71.
16. Bhat Y R, Lewis LE, Ke V. Bacterial isolates of early-onset neonatal sepsis and their antibiotic susceptibility pattern between 1998 and 2004: An audit from a center in India. Italian J Pediatr2011; 37:32doi: 10.1186/1824-7288-37-32. [PubMed]
17. Van den Hoogen A, Gerards LJ, Verboon-Maciolek MA, Fleer A, Krediet TG. Long-term trends in the epidemiology of neonatal sepsis and antibiotic susceptibility of causative agents. Neonatology 2010; 97:22-8.
18. Agnihotri N, Kaistha N, Gupta V. Antimicrobial susceptibility of isolates from neonatal septicemia. Jpn J Infect Dis 2004; 57:273-5.
19. Gerdes JS. Diagnosis and management of bacterial infections in the neonate. Paeditr Clin North Am 2004 Aug; 51(4):939-59. [PubMed]
20. Sriram R. Correlation of blood culture results with the sepsis score and the sepsis screen in the diagnosis of neonatal septicemia. Int J Biol Med Res. 2011; 2(1): 360-68.
21. Swarnakar K, Swarnakar M. A study of early onset neonatal sepsis with special reference to sepsis screening parameters in a tertiary care centre of rural India. The Internet J Inf Dis. 2012 ;10(1).
22. Jadhav S, Misra R, Vyawahare C, Angadi K, Gandham N, Ghosh P. Role of sepsis screen in the diagnosis of neonatal sepsis. Medical Journal of Dr DY Patil University. 2013;6(3):254-57.
23. Vinay BS, Girish G N, Adhikari S, Hugara S. Evaluation of septic screen as a diagnostic tool for neonatal sepsis in a tertiary hospital at Mysore. Sch J App Med Sci. 2015;3(2G):1005-10.
24. Bhale CP, Kale AV, Kale SS, Mahajan S, Mulay SS. Utility of Sepsis Screen in the Early Diagnosis of Neonatal Sepsis. Indian Journal of Neonatal Medicine and Research. 2016 July, Vol-4(3): IO01-IO07.
Copyright (c) 2018 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


