Study of cranial ultrasound its correlation with perinatal risk factors and its outcome in preterm neonates admitted to Neonatal intensive care unit
Abstract
Aims and Objectives: To determine the frequency of cranial ultrasound abnormalities in preterm neonates in the first week of life. To evaluate the association between cranial ultrasound findings and perinatal risk factors in regard to the immediate clinical outcome.
Materials and Methods: This Retrospective study was done in NICU in a tertiary hospital. Records of all preterm neonates (<37weeks) admitted to NICU who underwent neuro-sonography between Jan2016 – Jan2017 were included.
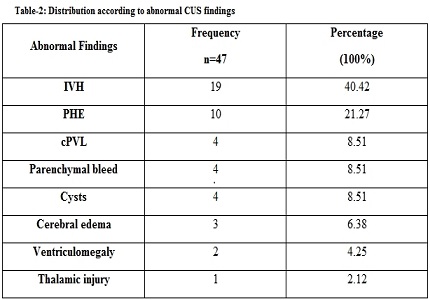
Results: Out of 100 preterms, 53% had normal CUS findings while 47% had abnormal finding. Abnormal CUS was significantly associated with gestational age <32weeks (p<0.001) and birth weight <1.5kg (p=0.006).Among the abnormal CUS findings intraventricular hemorrhage was the most common (40.42%) followed by periventricular hyper-echogenicity (21.27%), cystic periventricular leukomalacia (8.51%), parenchymal bleed (8.51%), cysts (8.51%), cerebral edema (6.38%), ventriculomegaly (4.25%) and thalamic injury (2.12%). Neonatal comorbidities associated with abnormal cranial ultrasound were RDS (25.53%), neonatal sepsis (21.27%), birth asphyxia (17.02%), neonatal seizures (8.51%), NEC (6.38%) and others (21.27%). There was significant association between abnormal cranial ultrasound and RDS (p=0.014) and birth asphyxia (p=0.008). Mortality was 36.1% and all had abnormal cranial USG. Intraventricular hemorrhage (76.4%) was the most common cause of death followed by parenchymal bleed (11.7%).
Conclusion: There was significant association between abnormal CUS and gestational age and birth weight. Most common abnormality was IVH and it carried the highest mortality. RDS and birth asphyxia had significant association with abnormal ultrasound. Early neurosonography could help in prognosticating immediate outcome and early intervention.
Downloads
References
2. Canadian Paediatric Society Statement. Routine screening cranial ultrasound examinations for the prediction of long-term neurodevelopmental outcomes in preterm infants. Paediatr Child Health. 2001;6(1):39-43.
3. Ghoor A, Scher G, Ballot DE. Prevalence of and risk for cranial ultrasound abnormalities in very-low-birth-weight infants at Charlotte Maxeke Johannesburg academic hospital. S Afr J Child Health 2017;11(2):66-70.
4. Thompson DK, Warfield SK, Carlin JB, et al. Perinatal risk factors altering regional brain structure in preterm infant. Brain 2007;130(3):667-677. Doi:10.1093/brain/awl277.
5. Nagraj N, Berwal PK, Srinivas A, et al. A study of neurosonogram abnormalities, clinical correlation with neurosonogram findings, and immediate outcome of high-risk neonate in neonatal intensive care unit. J PediatrNeurosci2016;11:200-5.
6. Poornima Shankar, Nithya S.L. Role of cranial ultrasound in high risk neonates in NICU. J of Evolution Med and Dent Sci 2014;3(15);3970-3976.
7. Gerda van Wezel-Meijler. Cranial Ultrasonography: advantages and aims part 1, Neonatal Cranial ultrasonography, 1st edition. Berlin:Springer, 2007:pg 3-4.
8. Prithviraj D, Reddy B, Shruthi B. Neurosonogram in critically ill neonates in neonatal intensive care unit. Int J Sci Stud 2016;4(1):124-128. [PubMed]
9. de Vries LS, Groenendaal F. Neuroimaging in preterm infants. Ment Retard Dev DisabilRes Rev 2002;8(4):273-80. Doi:10.1002/mrdd.10050. [PubMed]
10. Daneman A, Epelman M, Blaser S, Jarrin JR. Imaging of the brain in full-term neonates: does sonography still play a role? PediatrRadiol. 2006 Jul;36(7):636-46. Epub 2006 May 16. [PubMed]
11. de Vries LS, Cowan FM. Should cranial MRI screening of preterm infants become routine? Nat Clin Pract Neurol. 2007 Oct;3(10):532-3. Epub 2007 Aug 28. [PubMed]
12. Tann CJ, Nakakeeto M, Hagmann C, et al. Early cranial ultrasound findings among infants with neonatal encephalopathy in Uganda: an observational study. Pediatric RESEARCH 2016;80(2):190-196.
13. Leijser LM, Vein AA, Liauw L, Strauss T, Veen S, Wezel-MeijlerGv. Prediction of short-termneurologicaloutcome in full-termneonates with hypoxic-ischaemic encephalopathybased on combined use of electroencephalogram and neuro-imaging.Neuropediatrics. 2007 Oct;38(5):219-27. doi: 10.1055/s-2007-992815. [PubMed]
14. Bradway N, Edrees A, Sebaie DE, et al. Cranial ultrasonographic screening of the preterm newborn. Alex J Pediatr 2005;19(2):347-356.
15. Jha R, Singh A, Jha R. Cranial ultrasound in high risk preterm. New Indian Journal of Pediatrics 2017;6:26-32.
16. Boal DK, Watterberg KL, Miles S, et al. Optimal cost-effective timing of cranial ultrasound screening in low birth weight infants. PediatrRadiol 1995;25(6):425-8. PubMed PMID: 7491190. [PubMed]
17. Nagraj N, Berwal PK, Choudhary S. A prospective study of correlation of gestational age, birth weight and perinatal risk factors with various cranial ultrasound findings in high risk neonates. Indian Journal of Neurosciences 2016;2(2):43-45.
18. Vermeulen GM, Bruinse HW, Gerards LJ, et al. Perinatal risk factors for cranial ultrasound abnormalities in neonates born after spontaneous labour before 34 weeks. Eur J Obstetrics Gynecology Reprod Biol 2001;94(2):290-295. [PubMed]
19. Ballabh P. Pathogenesis and prevention of intraventricularhemorrhage. Clin Perinatol. 2014 Mar;41(1):47-67. doi: 10.1016/j.clp.2013.09.007. Epub 2013 Dec 12.
20. Mulindwa MJ, Sinyangwe S, Chomba E. The prevalence of intraventricular hemorrhage and associated risk factors in preterm neonates in the neonatal intensive care unit at the University teaching hospital, Lusaka, Zambia. Med J Zambia 2012;39(1):1-6.
Copyright (c) 2018 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


