Clinico-laboratory profile and mortality in plasmodium falciparum and vivax malaria in a tertiary centre
Abstract
Introduction: Malaria is a disease of global health importance and currently, 95% of the Indian population lives in malaria endemic area. Malaria parasite profile has been changing significantly over the years and is responsible for significant mortality and morbidity.
Objective: To study the clinic-hematological profile and mortality in plasmodium vivax and falciparum malaria.
Methodology: Hospital based observational study in a tertiary care centre for a period of 4 years including children <14 years of age who were tested positive for plasmodium vivax/falciparum.
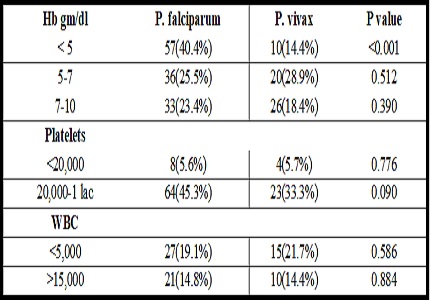
Results: A total of 230 confirmed cases of malaria were taken up, of which 141 were P. falciparum (61.30%) and 69 were P. vivax (30%) positive. 20 patients were positive for both Pf and Pv (8.70%). Fever with chills and/or rigor was most common symptom and pallor followed by splenomegaly was the most common physical signs. The most common hematological abnormality noted was anemia followed by thrombocytopenia. Anemia was more common in p. falciparum and in children below 5 years of age. Mortality was highest in p. falciparum malaria (5.67%) followed by mixed infection (5%) and Pv (2.89%). Cerebral malaria was most common cause of mortality (6 cases) followed by acute renal failure and shock. Complications were more common with Pf group, though they were also seen in Pv group.
Conclusion: Cerebral malaria is the most lethal entity of severe malaria and children are more prone than other susceptible groups. Encephalopathy, shock and renal failure at the time of presentation were poor prognostic factors, while anemia and thrombocytopenia were not found to be associated with adverse outcome.
Downloads
References
2. National Vector Borne Disease Control Programme (NVBDCP). [Internet]. [Updated 2013 May30; cited 2018 Feb10]. Available from: http://www.health.mp.gov.in/malaria.htm
3. Singh N, Dash AP, Thimasarn K. Fighting malaria in Madhya Pradesh (Central India): are we losing the battle? Malar J. 2009 May 7;8:93. doi: 10.1186/1475-2875-8-93.
4. Singh N, Dash AP, Varun BM, Kataria OM. Tribal Malaria. ICMR Bulletin. 2004; 34:1-10.
5. Yadav D, Chandra J, Dutta AK. Benign tertian malaria: how benign is it today? Indian J Pediatr. 2012 Apr;79(4):525-7. doi: 10.1007/s12098-011-0514-x. Epub 2011 Jun 25. [PubMed]
6. Genton B, D’Acremont V, Rare L, BaeaK, Reeder JC, AlpersMP, et al. Plasmodium vivax and mixed infections are associated with severe malaria in children: a prospective cohort study from Papua New Guinea. PLos Med. 2008 Jun 17; 5 (6): e127. doi:10.1371/journal.pmed.0050127. [PubMed].
7. Kumar A, Valecha N, Jain T, Dash AP. Burden of malaria in India: retrospective and prospective view. Am J Trop Med Hyg. 2007 Dec;77 (6 suppl):69–78. doi: 10.4269/ajtmh.2007.77.69.
8. Hazra BR, Chowdhury RS, Saha SK, Ghosh MB, Mazumder AK. Changing scenario of malaria: a study at Calcutta. Indian J Malariol. 1998 Jun; 35(2):111-6. [PubMed]
9. Patel DN, Pradeep P, Surti MM, Agarwal SB. Clinical manifestations of complicated Malaria- an overview. JIACM. 2003; 4(4):323-31. [PubMed]
10.Yadav D, Chandra J, Aneja S, Kumar V, Kumar P, Dutta AK. Changing profile of severe malaria in north Indian children. Indian J Pediatr. 2012 Apr;79(4):483-7. doi: 10.1007/s12098-011-0603-x. Epub 2011 Nov 18.
11. Kochar DK, Tanwar GS, Khatri PC, Kochar SK, Sengar GS, Gupta A et al. Clinical features of children hospitalized with malaria- a study from Bikaner, northwest India. Am J Trop Med Hyg. 2010;83:981–9. doi: 10.4269/ajtmh.2010.09-0633.[ PMC free article] [PubMed]
12. Parakh A, Agarwal N, Aggarwal A, Aneja A. Plasmodium vivax malaria in children : uncommon manifestations. Ann Trop Pediatr. 2009; 29 (4):253–6.doi: 10.1179/027249309X12547917868844. [PubMed]
13. Price RN, Simpson JA, Nosten F, Luxemburger C, Hkirjaroen L, ter Kuile F, Chongsuphajaisiddhi T, White NJ. Factors contributing to anemia after uncomplicated falciparum malaria. Am J Trop Med Hyg. 2001 Nov;65(5):614-22. [PubMed]
14. Sharma SK, Das RK, Das BK, Das PK. Haematological and coagulation profile in acute falciparum malaria. J Assoc Physicians India. 1992 Sep;40(9):581-3. [PubMed]
15. Perrin LH, Mackey LJ, Miescher PA. The hematology of malaria in man. Semin Hematol. 1982 Apr;19(2):70-82. [PubMed]
16. Jadhav UM, Patkar VS, Kadam NN. Thrombocytopenia in malaria--correlation with type and severity of malaria. J Assoc Physicians India. 2004 Aug;52:615-8.
17. Rodrıguez-Morales AJ, Sanchez E, Vargas M, Piccolo C, Colina R, Arria M. Anemia and thrombocytopenia in children with plasmodium vivax malaria. J Trop Pediatr. 2006 Feb;52 (1):49–51. doi: 10.1093/tropej/fmi069.
18. Kochar DK, Das A, Kochar SK, Saxena V, Sirohi P, Garg S, Kochar A, Khatri MP, Gupta V. Severe Plasmodium vivax malaria: a report on serial cases from Bikaner in northwestern India. Am J Trop Med Hyg. 2009 Feb;80(2):194-8. [PubMed]
19. Krishnan A, Karnad DR. Severe falciparum malaria: an important cause of multiple organ failure in Indian intensive care unit patients. Crit Care Med. 2003 Sep;31(9):2278-84. [PubMed]
20. Erhart LM, Yingyuen K, Chuanak N, Buathong N, Laoboonchai A, Miller RS, Meshnick SR, Gasser RA Jr, Wongsrichanalai C. Hematologic and clinical indices of malaria in a semi-immune population of western Thailand. Am J Trop Med Hyg. 2004 Jan;70(1):8-14. [PubMed]
21. Mishra SK, Mahanta KC, Mohanty S. Malaria associated acute renal failure--experience from Rourkela, eastern India. J Indian Med Assoc. 2008 Oct;106(10):640-2, 654. [PubMed]
22. Severe falciparum malaria. World Health Organization, Communicable Diseases Cluster. Trans R Soc Trop Med Hyg. 2000 Apr;94 Suppl 1:S1-90.
23. Nand N, Aggrawal H, Sharma M, Singh M. Systemic manifestations of malaria. Journal,Indian academy of clinical medicine. 2001Jul- Sept; 2 (3): 189-94.
24. Price RN, Douglas NM, Anstey NM. New developments in Plasmodium vivax malaria: severe disease and the rise of chloroquine resistance. Curr Opin Infect Dis. 2009 Oct;22(5):430-5. doi: 10.1097/QCO.0b013e32832f14c1. [PubMed]
25. Luxemburger C, Ricci F, Nosten F, Raimond D, Bathet S, White NJ. The epidemiology of severe malaria in an area of low transmission in Thailand. Trans R Soc Trop Med Hyg. 1997 May-Jun;91(3):256-62. [PubMed]
26. Maitland K, Williams TN, Newbold CI. Plasmodium vevax and P.falciparum: Biological interactions and the possibility of cross-species immunity. Parasitol Today. 1997 Jun; 13 (6):227–31. [PubMed]
27. Tjitra E, Anstey NM, Sugiarto P, Warikar N, Kenangalem E, Karyana M, Lampah DA, Price RN. Multidrug-resistant Plasmodium vivax associated with severe and fatal malaria: a prospective study in Papua, Indonesia. PLoS Med. 2008 Jun 17;5(6):e128. doi: 10.1371/journal.pmed.0050128. [PubMed]
Copyright (c) 2018 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


