A study of clinical and laboratory profiles of dengue fever in children
Abstract
Background: Early recognition of characteristic clinical and laboratory parameters of is importantto facilitate prompt diagnosis andtreatmentfor a better outcome, particularly in dengue burden countries.
Methods: Children aged less than 15 years who sought medical care in the pediatric department of Saveetha medical college, diagnosed as Probable Dengue/Dengue fever/ dengue with warning sign/severe dengue according to standard guidelines during the study period (July 2017 – December 2017) comprised the study sample.
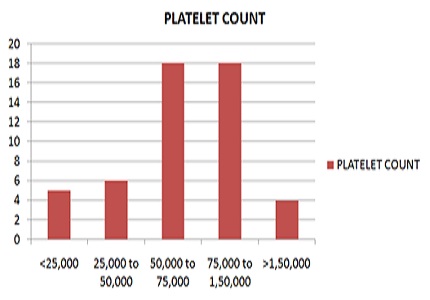
Results: A total of 61 cases were enrolled, of these 36 were boys. The mean age was 6.49 years. Only five patients had severe dengue. Fever(96.7%), loss of appetite (59%), cough and running nose (33%) were common symptoms noted and itching (37.7%) was common during recovery. Only 11.4% of children had bleeding manifestation. Hepatomegaly was noticed in 35 children. Five children went into shock, 2 of whom had hypotension. NS1 was positive in 49%, IgM in 36%, and IgG in 13%. NS1 positivity rate on day 4, day 5 and day 6 of illness were 62.5%, 38.4% and 18.1% respectively.
Conclusion: Dengue fever is common during monsoon season, and the course and severity are highly variable. Though the manifestations of dengue are similar to other viral infections, morbidity and mortality are more, thus requiring early diagnosis. As observed in our study the presence of prodromal respiratory symptoms does not preclude the diagnosis of dengue. There should be a high index of suspicion of co-infection, notablymalaria and scrub typhus, if there is an unusual persistence of fever.
Downloads
References
2. Verhagen LM, de Groot R. Dengue in children. J Infect. 2014 Nov;69 Suppl 1:S77-86. doi: 10.1016/j.jinf.2014. 07.020. Epub 2014 Sep 13. [PubMed]
3. Bhatt S, Gething PW, Brady OJ, Messina JP, Farlow AW, Moyes CL, Drake JM, Brownstein JS, Hoen AG, Sankoh O, Myers MF, George DB, Jaenisch T, Wint GR, Simmons CP, Scott TW, Farrar JJ, Hay SI. The global distribution and burden of dengue. Nature. 2013 Apr 25;496(7446):504-7. doi: 10.1038/nature12060. Epub 2013 Apr 7.
4. Mutheneni SR, Morse AP, Caminade C, Upadhyayula SM. Dengue burden in India: recent trends and importance of climatic parameters. Emerg Microbes Infect. 2017 Aug 9;
6(8):e70.doi: 10.1038/emi.2017.57. [PubMed]
5. Kakkar M.Dengue fever is massively under-reported in India, hampering our response.BMJ. 2012 Dec 19; 345: e8574. doi: 10.1136/bmj.e8574. [PubMed]
6. Chakravarti A, Arora R, Luxemburger C. Fifty years of dengue in India. Trans R Soc Trop Med Hyg. 2012 May; 106 (5):273-82. doi: 10.1016/j.trstmh.2011.12.007. Epub 2012 Feb 21. [PubMed]
7. Hermann LL, Gupta SB, Manoff SB, Kalayanarooj S, Gibbons RV, Coller BA. Advances in the under standing, management, and prevention of dengue. J Clin Virol. 2015 Mar;64:153-9. doi: 10.1016/j. jcv.2014. 08.031. Epub 2014 Oct 20.
8. Mørch K, Manoharan A, Chandy S, Chacko N, Alvarez-Uria G, Patil S, et al. Acute undifferentiated fever in India: a multicentre study of aetiology and diagnostic accuracy.
BMC Infect Dis. 2017 Oct 4; 17(1):665.doi: 10.1186/s12879-017-2764-3. [PubMed]
9. Trang NTH, Long NP, Hue TTM, Hung LP, Trung TD, Dinh DN, Luan NT, Huy NT, Hirayama K. Association between nutritional status and dengue infection: a systematic review and meta-analysis. BMC Infect Dis. 2016 Apr 20;16:172. doi: 10.1186/s12879-016-1498-y. [PubMed]
10. Hansen C, Paintsil E.Infectious Diseases of Poverty in Children: A Tale of Two Worlds. Pediatr Clin North Am. 2016 Feb;63(1):37-66. doi: 10.1016/j.pcl.2015.08.002. [PubMed]
11. Daudé É, Mazumdar S, Solanki V. Widespread fear of dengue transmission but poor practices of dengue prevention: A study in the slums of Delhi, India. PLoS One. 2017 Feb 10;12(2):e0171543. doi: 10.1371/journal.pone.0171543. eCollection 2017. [PubMed]
12. Giersing BK, Modjarrad K, Kaslow DC, Moorthy VS; WHO Product Development for Vaccines Advisory Committee; WHO Product Development for Vaccines Product Development Advisory Committee:. Report from the World Health Organization's Product Development for Vaccines Advisory Committee (PDVAC) meeting, Geneva, 7-9th Sep 2015. Vaccine. 2016 Jun 3;34(26):2865-2869. doi: 10.1016/j.vaccine.2016.02.078. Epub 2016 Mar 15. [PubMed]
13. Malisheni M Khaiboullina SF, Rizvanov AA Takah N, Murewanhema G, Bates M. Clinical Efficacy, Safety, and Immunogenicity of a Live Attenuated Tetravalent Dengue Vaccine (CYD-TDV) in Children: A Systematic Review with Meta-analysis. Front Immunol. 2017 Aug 4;8:863. doi: 10.3389/fimmu.2017.00863. eCollection 2017.
14. Guidelines on Clinical Management of Dengue Fever and Dengue Haemorrhagic Fever. The government of India. Directorate of National Vector Borne Diseases Control Programme. Directorate General of Health Services, Ministry of Health and Family Welfare. National Vector Borne Disease Control Programme (NVBDCP).
15. Pothapregada S, Kamalakannan B, Thulasingham M, Sampath S. Clinically Profiling Pediatric Patients with Dengue. J Glob Infect Dis. 2016 Jul-Sep;8(3):115-20. doi: 10.4103/0974-777X.188596.
16. Sharma NL, Balasubramanyam V, Kandati J, Ponugoti M. Clinical and laboratory profile of dengue fever in children during an outbreak - one year study at tertiary care hospital, Chennai, Tamilnadu, India. Int J Contemp Pediatr2017;4:110-5.doi: 10.4103/ijmr.IJMR_1325_16.
17. Ramabhatta S, Palaniappan S, Hanumantharayappa N, Begum SV. The Clinical and Serological Profile of Pediatric Dengue. Indian J Pediatr.2017 Dec;84(12):897-901.doi:10.1007/s12098-017-2423-0. Epub 2017Sep 8. [PubMed]
18. Aggarwal A, Chandra J, Aneja S, Patwari AK, Dutta AK. An epidemic of dengue hemorrhagic fever and dengue shock syndrome in children in Delhi.Indian Pediatr. 1998 Aug;35(8):727-32. [PubMed]
19. Mishra S, Ramanathan R, Agarwal SK. Clinical profile of dengue fever in children: a study from Southern Odisha, India. Scientifica. 2016.doi: 10.1155/2016/6391594. [PubMed]
20. Kalayanarooj S, Vaughn DW, Nimmannitya S, Green S, Suntayakorn S, Kunentrasai N, Viramitrachai W, Ratanachu-eke S, Kiatpolpoj S, Innis BL, Rothman AL, Nisalak A, Ennis FA. Early clinical and laboratory indicators of acute dengue illness. J Infect Dis. 1997 Aug;176(2):313-21. [PubMed]
21. ABM Shahidul Alam, S Anwar Sadat, Zakaria Swapanet al. Clinical Profile of Dengue Fever in Children Bangladesh J child health 2009;33(2),55-8. doi: 10.3329/bjch.v33i2.5678.
22. Vijayalakshmi AM, Jayavardhana A. Febrile rash and convalescent rash of dengue fever. Indian Pediatr. 2013 Jul;50(7):717. [PubMed]
23. Sahana KS1, Sujatha R. Clinical profile of dengue among children according to revised WHO classification: analysis of a 2012 outbreak from Southern India. Indian J Pediatr. 2015 Feb; 82(2):109-13. doi: 10.1007/s12098-014-1523-3.
24. PS Sahu, M Sahu, S Ambuet al. A review of concurrent infections of malaria and dengue in Asia. Asian Pac J Trop Biomed 6,2016 july ;6(7):633-8. doi: 10.1016/j.apjtb.2016.05.008.
25. Ahmed S, Arif F, Yahya Y, Rehman A, Abbas K, Ashraf S, Akram DS.Dengue fever outbreak in Karachi 2006--a study of profile and outcome of children under 15 years of age. J Pak Med Assoc. 2008 Jan;58(1):4-8. [PubMed]
26. Hari Kishan Jayanthi,Sai Krishna Tulasi. Correlation study between platelet count, leukocyte count, non-hemorrhagic complications, and duration of hospital stay in dengue fever with thrombocytopenia. J Family Med Prim Care. 2016 Jan-Mar; 5(1): 120–3. doi: 10.4103/2249-4863.184635.
Copyright (c) 2018 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


