Neonatal behavioral assessment among survivors of birth asphyxia using T.Berry Brazelton's NBAS
Abstract
Introduction: This study aims at providing baby-specific prognosisfor the survivors of birth asphyxia,regarding their neurological impairment, based on their behaviour assessment using T. BerryBrazelton′s NBAS.
Methods: 56 HIE survivors were randomly selected and grouped into 3 as HIE 1,2,3 based on Sarnat HIE staging. NBAS was scored just before discharge which consists of 28 behavior items & 7 supplementary items (9 points scale) and 18 reflex items (4-point scale). Scores calculated and compared between groups.
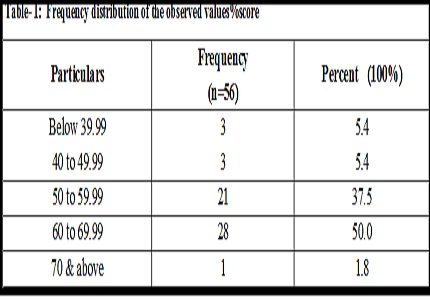
Results: The average score of HIE 1 babies were 65.01%, HIE 2 babies were 58.01% and that of HIE 3 babies were 41.75%. 60% of HIE 3 babies made a score less than 40 %. 73 % of HIE 2 babies scored between 50% and 60%. 88% of HIE 1 babies scored between 60% and 70%. More than 50% of HIE 1 babies had an abnormal reflex score less than 5 while more than 60% of HIE 2 babies scored between 6 and 10. HIE 3 were the worst to perform where 3 out of 5 babies scored >11. Sex of the babies, their birth weight and the mode of delivery showed no statistical significance for comparing them against the final % scores. Lower final scores were associated with higher abnormal reflex scores and vice versa.
Conclusions: NBAS helps us to prognosticate a baby individually rather than relying on past personal experience on the treating neonatologist or the available non-directive statistics. Every birth asphyxia survivor needs to be administered NBAS before discharge from hospital. By identifying the strength one can boost the mother's confidence in looking after the child and ease the rehabilitation and further intervention as would be required.
Downloads
References
2. Lawn JE, Blencowe H, Pattinson R, Cousens S, Kumar R, Ibiebele I, Gardosi J, Day LT, Stanton C; Lancet's Stillbirths Series steering committee. Stillbirths: Where? When? Why? How to make the data count?Lancet. 2011 Apr 23;377(9775):1448-63. doi: 10.1016/S0140-6736(10)62187-3. Epub 2011 Apr 13.
3. WHO. Perinatal Mortality: A Listing of Available Information. WHO; Geneva: 1996. WHO/FRH/MSM/96.7.
4. National neonatal perinatal database NNPD 2002-03. Indian Council of Medical Research, New Delhi. January 2005.
5. Use and abuse of the Apgar score. Committee on Fetus and Newborn, American Academy of Pediatrics, and Committee on Obstetric Practice, American College of Obstetricians and Gynecologists.Paediatrics.1996 Jul; 98(1):141-2.
6. MacLennan A. A template for defining a causal relation between acute intrapartum events and cerebral palsy: international consensus statement.BMJ.1999Oct16;319(7216):1054-9.
7. Peter Van Eerden, MD; Peter S. Bernstein Summary of the Publication. Neonatal Encephalopathy and Cerebral Palsy: Defining the Pathogenesis and Pathophysiology by the ACOG Task Force on Neonatal Encephalopathy and Cerebral Palsy July 03, 2003
8. Nageswara Prasad Vunnava. Chap 28.Essentials of Neonatal Emergencies and Clinical Guidelines Paperback – 31 Jan 2013.
9. SarnatHB, Sarnat MS. Neonatal encephalopathy following fetal distress. A clinical and electro encephalo graphic study. Arch Neurol.1976 Oct;33(10):696-705.
10. Levene MI. The asphyxiated newborn. In.: Levene MI, Lilford RJ. F et al and neonatal neurology and neurosurgery. Edinburg: Churchill livingstone1995;405-26.
11. Thompson CM, Puterman AS, Linley LL, Hann FM, van der Elst CW, Molteno CD, Malan AF. The value of a scoring system for hypoxic ischaemic encephalopathy in predicting neuro developmental outcome. Acta Paediatr. 1997 Jul;86(7):757-61.
12. Robertson CM, Finer NN. Long-term follow-up of term neonates with perinatal asphyxia.Clin Perinatol. 1993 Jun; 20(2):483-500. [PubMed]
13. John P Cloherty, Lippincott Williams &Wilkins. Manual of neonatal care 7 theditionChap55,25-26.
14. Brazelton, T. Berry; Nugent, J. Kevin. Neonatal behavioral assessment scale (4th ed.). London: Mac Keith Press. ISBN 978-1-907655-03-6.oct 2011.
15. Lester et al (1982 ,84 ). Lester BM. Data analysis and prediction. In: Brazelton TB, Neonatal behavioral assessment scale 2nd ed, London, Mac Keith Press.
16. Black M, Schuler M, Nair P. Prenatal drug exposure : neurodevelopmental outcome and parenting environment. J Pediatr Psychol. 1993 Oct; 18(5): 605–620.
17. Mansi G, Raimondi F, Pichini S, Capasso L, Sarno M, Zuccaro P, Pacifici R, Garcia-Algar O, Romano A, Paludetto R. Neonatal urinary continence correlates with behavioral alterations with newborns prenatally exposed to tobacco smoke. Pediatr Res. 2007 Feb;61(2):257-61.
18. Tim F. Oberlander, Sandra W. Jacobson, Joanne Weinberg, Ruth E. Grunau, Christopher D. Molteno, and Joseph L. Jacobson. Prenatal alcohol exposure alters behavioural reactivity to pain in newborns. Alcohol clin exp res 34:681-692. Published online 2010 Jan 27. doi: 10.1111/j.1530-0277.2009.01137.x
19. Tronic EZ. The Neurobehavioral and Social-Emotional Development of Infants and Children Ed Tronick, W. W. Norton & Company: New York, NY, 2007. 571 pp, CA $68.00.J Can Acad Child Adolesc Psychiatry. 2009 Aug; 18(3): 263–264.
Copyright (c) 2018 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


