Correlation of financial burden with severity of asthma in children
Abstract
Introduction: Urbanisation is causing a rise in the financial burden of Asthma in children and it varies with the disease severity. Asthma has a low public health priority and is often under diagnosed and treated inappropriately.
Objectives: Our aim was to correlate the financial burden of disease costs with Asthma classification.
Methods: It was a prospective study of 38 patients attending paediatric pulmonology clinic in a tertiary care hospital. Details were entered in a predesigned proforma and institutional ethics committee approval was taken. Quantitative statistical analysis using mean, standard deviation and applying one way ANNOVA test was done.
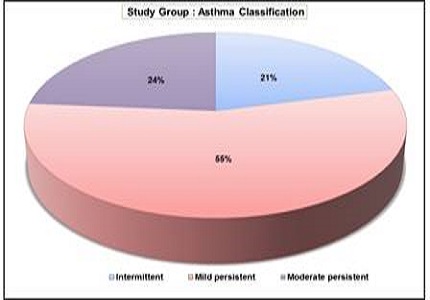
Results: Intermittent, mild and moderate persistent asthma were 8 (21.05%), 21(55.26%) and 9(23.68%) respectively. Majority of the patients;19 (50%) belonged to the upper middle class.The direct mean costs across severities ranged between INR 5700-7400 for general practitioner consultation, INR 3550-10300 for emergency visits, INR 4500-9000 for investigations and INR 7000-13700 for medications. The indirect costs ranged between INR 9000-19800 on daily wages lost, INR 2900-8700 on travel expenses (significant p value<0.014) between mild and moderate persistent asthma. Mean costs on food ranged between INR 1700-3200, tuitions INR 3000-5700 and miscellaneous expenditure being INR 2000-8300.The percentage of annual income spent was 28.76%, 40.99% and 60.64% in intermittent, mild and moderate persistent asthma respectively.
Conclusion: Early referral, diligent counselling, physician and parents education along with good compliance would impart effective control and thereby reduce economic burden.
Downloads
References
2. Riccioni G, D'Orazio N, Di Ilio C, Menna V, Guagnano MT, Della Vecchia R. Quality of Life and clinical symptoms in asthmatic subjects. J Asthma. 2004 Feb; 41 (1): 85-9.
3. Gergen PJ: Understanding the economic burden of asthma. J Allergy ClinImmunol 2001. 107(5): 5445-5448.
4. Braman SS. The global burden of asthma. Chest. 2006 Jul;130(1 Suppl): 4S-12S.
5. Vos T, Flaxman AD, Naghavi M, Lozano R et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012 Dec 15;380 (9859): 2163-96. doi: 10.1016/S0140-6736(12)61729-2. [PubMed]
6. Fowler MG, Davenport MG, Garg R. School functioning of US children with asthma.Pediatrics. 1992 Dec;90 (6): 939-44.
7. Grupp-Phelan J, Lozano P, Fishman P. Health care utilization and cost in children with asthma and selected comorbidities. J Asthma. 2001 Jun;38(4):363-73.
8. Gupta RS, Bewtra M, Prosser LA, Finkelstein JA.Predictors of hospital charges for children admitted with asthma. Ambul Pediatr. 2006 Jan-Feb; 6(1):15-20.
9. Agrawal S, Pearce N, Ebrahim S. Prevalence and risk factors for self-reported asthma in an adult Indian population: a cross-sectional survey. Int J Tuberc Lung Dis. 2013 Feb;17(2):275-82. doi: 10.5588/ijtld.12.0438. [PubMed]
10. Agnihotram R, and Chattopadhyay A. Respiratory Disease Burden In Rural India: A Review From Multiple Data Sources, Internet J. Epidemiol, 2005; vol 2, no.2.
11. Ford ES, Mannino DM, Homa DM, Gwynn C, Redd SC, Moriarty DG, et al. Self-reported asthma and health-related quality of life: findings from the behavioral risk factor surveillance system. Chest. 2003 Jan;123(1):119-27. [PubMed]
2. Bahadori K, Doyle-Waters MM, Marra C, Lynd L, Alasaly K, Swiston J, et al. Economic burden of asthma: a systematic review. BMC Pulm Med. 2009 May 19;9:24. doi: 10.1186/1471-2466-9-24.
13. Sharifi L, Dashti R, Pourpak Z, Fazlollahi MR, Movahedi M, Chavoshzadeh Z, et al. Economic Burden of Pediatric Asthma: Annual Cost of Disease in Iran. Iran J Public Health. 2018 Feb;47(2):256-263. [PubMed]
14. Dashti R, Sedighy M, Pourpak Z, Ahmadiani MS, Fazlollahi MR, Bavarian B, et al.Direct economic cost of acute asthma in emergency department. Indian J Pediatr. 2013 Aug;80(8):708-9. doi: 10.1007/s12098-012-0912-8. Epub 2012 Nov 24.
15. Kauppi P, Linna M, Martikainen J, Mäkelä MJ, Haahtela T. Follow-up of the Finnish Asthma Programme 2000-2010: reduction of hospital burden needs riskgroup rethinking.Thorax. 2013Mar;68(3):292-3.doi: 10.1136/ thoraxjnl -2011-201028. Epub 2012 Apr 15. [PubMed]
16. Wang LY, Zhong Y, Wheeler L. Direct and indirect costs of asthma in school-age children. Prev Chronic Dis. 2005 Jan; 2 (1):A11. Epub 2004 Dec 15. [PubMed]
17. Cisternas MG, Blanc PD, Yen IH, Katz PP, Earnest G, Eisner MD, et al. A comprehensive study of the direct and indirect costs of adult asthma. J Allergy Clin Immunol. 2003 Jun;111(6):1212-8. [PubMed]
18. Ungar WJ, Coyte PC; Pharmacy Medication Monitoring Program Advisory Board. Prospective study of the patient-level cost of asthma care in children. Pediatr Pulmonol. 2001 Aug; 32 (2):101-8. [PubMed]
19. Shafazand S, Colice G.Asthma: the epidemic has ended, or has it? Chest. 2004 Jun;125(6):1969-70. [PubMed]
20. Matricardi PM, Bonini S. Why is the incidence of asthma increasing? In: Johnston SL, Holgate ST(eds). Asthma: Critical Debates. London: Blackwell Science; 2002:3-17.
Copyright (c) 2018 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


