Bacterial sensitivity pattern of neonatal early onset sepsis in a tertiary care hospital in Assam
Abstract
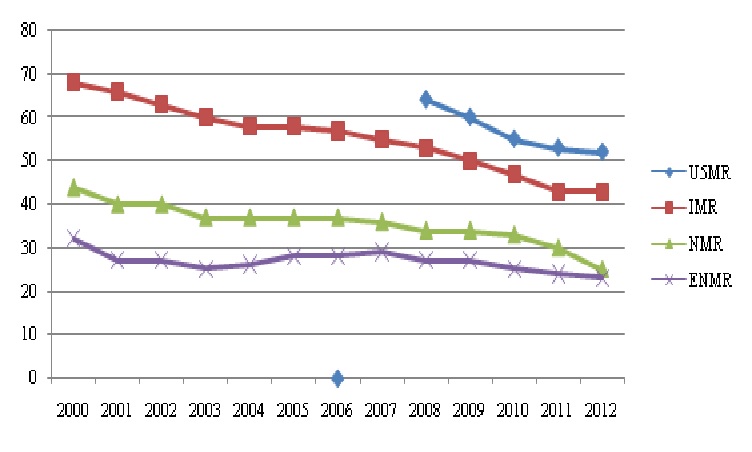
Introduction: Current trend in Neonatal mortality rate (NMR) is stagnant for last few decades. Early onset sepsisis one of commonest causes of NMR. As clinical presentation is often nonspecific, a high degree of suspicion is required for early initiation of specific therapy. Choice of empiricalantibiotic is the cornerstone of specific therapy. Depending on the culture report it can be switched over to appropriate antibiotic. Prevalence of bacterial pathogen varies in different locality. So, every neonatal care set up should have a periodical review of the bacteriological profile of the locality.
Method: A prospective cohort study was undertaken in the department of Pediatrics and Obstetrics of Tezpur Medical College and hospital, Assam to find out the bacteriological profile of culture proven early onset sepsis (EOS) during July 2016 to June 2017.
Results: Out of 5960 hospital born babies, 298 babies fulfilled the inclusion and exclusion criteria. 15(5.03 %) babieswere with probable sepsis by clinical criteria and positive sepsis screen. Out of these, 7(46.66 %) babies were culture positive. Gram negative organisms were 85.7 % of isolates of which 3(42.8%) were Actinobacterspp followed by klebseilla, E. Coli and Pseudomonus Aeroginosa. Methicillin resistant Staph aureus was the only gram-positive organism. There was no growth of group B streptococcus. Most of the organisms were resistant to common drugs. One of Actinobacter was resistant to all drugs including meropenam.
Conclusion: We conclude that only local policy of rational antibiotic use can prevent the problem of drug resistance and reduce NMR due to sepsis.
Downloads
References
2. Pawa AK, Ramji S, Rakish K, Thirupuram S. Neonatal nosocomial infections: profile and risk factors. India J Paediatr. 1997;34:297-302.[pubmed]
3. Agarwal R, Sarkar N, Deorary AK, Paul VK. Sepsis in Newborn. Indian J Pediatr. 2003;68:528-37.[pubmed]
4. Sankar MJ, Agarwal R, Deorari AK, Paul VK. Sepsis in the newborn. Indian J Pediatr. 2008 Mar;75(3):261-6.[pubmed]
5. Dadhich JP, Paul VK. State of India’s Newborns, National Neonatology Forum and Saving Newborn Lives. New Delhi. Save the Children (US); 2004.
6. Stoll BJ. The global impact of neonatal infection. Clin Perinatol. 1997 Mar;24(1):1-21.[pubmed]
7. National Neonatal Perinatal Database. Report for year 2002-2003. National Neonatology Forum. India; 2005 Jan. www.newbornwhocc.org
8. Meharbansingh. Care of The Newborn. 7th Edition. Sagar Publishers; 2010. P.2-3.
9.Leung WS, Chu CM, Tsang KY, et al. Fulminant community-acquired Acinetobacter baumannii pneumonia as a distinct clinicalsyndrome. Chest. 2006 Jan;129(1):102-9. doi:10.1378/chest.129.1.102
10. Chacko B, Sohi I. Early onset neonatal sepsis. Indian J Pediatr. 2005 Jan;72(1):23-6.[pubmed]
11. Twinkle N Gandhi et al. Utility of c reactive protein as inflammatory marker in early diagnosis of neonatal septicaemia: a cross sectional study, national journal of medical research. 2012 Oct – Dec; Volume2│Issue 4│
12. Sucilathangam G et al. Diagnostic value of C-reactive protein and haematological markers in neonatal sepsis. Gomal J Med Sci. 2013; 11:212-215.[pubmed]
13. Hari PN et al. Bacteriological profile of neonatal septicemia cases and the antimicrobial resistance pattern in a tertiary care hospital of central Nepal. IJBAR. 2013; 04 (01)
14. Bhat Y R, Lewis LE, K E V.Bacterial isolates of early-onset neonatal sepsis and their antibiotic susceptibility pattern between 1998 and 2004: an audit from a center in India. Ital J Pediatr. 2011 Jul 11;37:32. doi: 10.1186/1824-7288-37-32.[pubmed]
15. Shah BA, Padbury JF. Neonatal sepsis: an old problem with new insights. Virulence. 2014 Jan 1;5(1):170-8. doi: 10.4161/viru.26906. Epub 2013 Nov 1.[pubmed]
16. Adair CE, Kowalsky L, Quon H, et al. Risk factors for early-onset group B streptococcal disease in neonates: a population-based case-control study. CMAJ. 2003 Aug 5;169(3):198-203.[pubmed]
17. Tita AT, Andrews WW. 2010. Diagnosis and management of clinical chorioamnionitis. Clin. Perinatol.37:339–354. 10.1016/j.clp.2010.02.003 [pubmed]
18. Arnon S, Litmanovitz I. Diagnostic tests in neonatal sepsis. CurrOpin Infect Dis. 2008 Jun;21(3):223-7. doi: 10.1097/QCO.0b013e3282fa15dd.[pubmed]
19. Anderson-Berry A. 2012. Neonatal sepsis. In Medscape reference. WebMD LLC, New York, NY:http://emedicine.medscape.com/article/978352-overview
Copyright (c) 2018 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


