Clinical profile of severe anemia in adolescents from a hilly terrain tertiary care hospital in north India
Abstract
Introduction: Adolescence is a vulnerable period for development of anemia. Anemia in adolescence has serious implications for a wide range of outcomes. It causes reduced resistance to infection, impaired physical growth and mental development, reduced physical fitness, work capacity and school performance.
Objectives: The aim of the present study was to study the clinical profile of the adolescents (10-18 years) admitted with severe anemia.
Methods: A hospital based retrospective study was conducted in the Department of Pediatrics, Dr Rajendra Prasad Government Medical College Kangra, a tertiary care institute in North India, during the period from January 2015 to December 2016. The participants in our study were the adolescent patients (10-18 years) admitted with primary diagnosis of severe anemia (Hemoglobin <7gm %). The diagnosis of type of anemia was based on hematological indices and red cell morphology on peripheral smear.
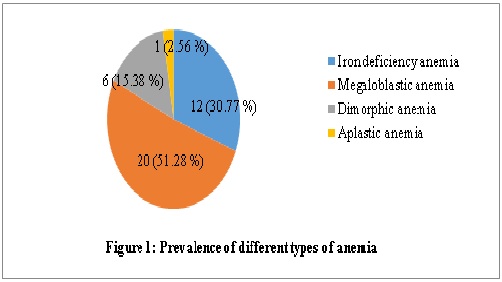
Results: There were 39 patients admitted with severe anemia. This constituted 1.90% of all the admissions during the study period. The mean age of the patients was 14.97 (± 1.86) years and the mean hemoglobin was 4.66 (± 1.28) gm%. There was a female preponderance with 66.67% females as against 33.33% males. Megaloblastic anemia was the most common type of anemia (52.28%) followed by iron deficiency anemia (30.77%) and dimorphic anemia (15.38%). All of the patients belonged to poor socioeconomic status and most of them (89.74%) were vegetarian.
Conclusion: Although iron deficiency anemia is the most common type of anemia in India, yet in adolescents megaloblastic and dimorphic anemia should be looked for whenever the adolescents present with severe anemia especially in the setting of malnutrition and dietary inadequacy.
Downloads
References
2. Kishore J. Editor. National Health Programs of India. 6th ed. New Delhi: Century Publications; 2006; 82-84.
3. Nayar PD, Mehta R. Child Health. In: Gupta P, Ghai OP, Editors. Textbook of Preventive and Social Medicine. 2nd ed. New Delhi: CBS Publishers and Distributors; 2007; 428-37.
4. Shobha S, Sharada D. Efficacy of twice weekly iron supplementation in anemic adolescent girls. Indian Pediatr. 2003 Dec;40(12):1186-90.[pubmed]
5. Choudhary A, Moses PD, Mony P, Mathai M. Prevalence of anaemia among adolescent girls in the urban slums of Vellore, south India. Trop Doct. 2006 Jul;36(3):167-9. doi:10.1258/004947506777978253
6. Roy S, Ray S. Prevention of malnutrition. J Indian Med Assoc. 2000 Sep;98(9):510-1.[pubmed]
7. Patra S, Pemde HK, Singh V, et al. Profile of adolescents with severe anemia admitted in a tertiary care hospital in northern India. Indian J Pediatr. 2011 Jul;78(7):863-5. doi: 10.1007/s12098-010-0336-2. Epub 2011 Jan 8.[pubmed]
8. Kapur D, Agarwal KN, Agarwal DK. Nutritional anemia and its control. Indian J Pediatr. 2002 Jul;69(7):607-16.[pubmed]
9. Chaudhary SM, Dhage VR. A study of anemia among adolescent females in the urban area of nagpur. Indian J Community Med. 2008 Oct;33(4):243-5. doi: 10.4103/0970-0218.43230.[pubmed]
10. Thomas D, Chandra J, Sharma S, et al. Determinants of Nutritional Anemia in Adolescents. Indian Pediatr. 2015 Oct;52(10):867-9.[pubmed]
11. Khanduri U, Sharma A, Joshi A. Occult cobalamin and folate deficiency in Indians. Natl Med J India. 2005 Jul-Aug;18(4):182-3.[pubmed]
12. Haq Salma, Iqbal Nasir, Fayyaz Fatima et al. Serum B12 and folate levels in patients with megaloblastic change in the bone marrow. Biomedica Vol. 28. Jan-June 2012; pp. 35-39.
13. Chhabra A, Chandar V, Gupta A, Chandra H. Megaloblastic anaemia in hospitalized children. Journal, Indian Academy of Clinical Medicine. 2012; 13(3): 195-7.
14. Viswanadham KK, Sahoo A. A study of clinical profile and factor associated with anemia in the school going children. International Medical Journal. September 2017; 4(a): 914-917.
15. Keikhaei B, Zandian K, Ghasemi A, Tabibi R. et al. Iron-deficiency anemia among children in southwest Iran. Food Nutr Bull. 2007 Dec;28(4):406-11. doi:10.1177/156482650702800405.[pubmed]
16. Dallman PR, Yip R, Johnson C. Prevalence and causes of anemia in the United States, 1976 to 1980. Am J Clin Nutr. 1984 Mar;39(3):437-45. doi:10.1093/ajcn/39.3.437.[pubmed]
17. Tolentino K, Friedman JF. An update on anemia in less developed countries. Am J Trop Med Hyg. 2007 Jul;77(1):44-51.[pubmed]
18. Balarajan Y, Ramakrishnan U, Ozaltin E, Anaemia in low-income and middle-income countries. Lancet. 2011 Dec 17;378(9809):2123-35. doi: 10.1016/S0140-6736(10)62304-5. Epub 2011 Aug 1.[pubmed]
19. Jain Neeraj, Jain Vibha Mangal. Prevalence of anemia in school children. Medical Practice and Review Feb 2012; Vol.3 (1):pp.1-4.
20. Verma M, Chhatwal J, Kaur G. et al. Prevalence of anemia among urban school children of Punjab. Indian Pediatr. 1998 Dec;35(12):1181-6.[pubmed]
21. Kakkar R, Kakkar M, Kandpal SD, Jethani S. Study of anemia in adolescent school girls of Bhopal. Indian J Community Health 2010; 22:38-40.
Copyright (c) 2018 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


