A study of facility and community phase management of children with Severe Acute Malnutrition at NRC in Central Gujarat
Abstract
Background:The burden of Severe Acute Malnutrition, Severe underweight, and stunting is-29.4%, 15.1% and 15%. The India National Family Health Survey (NFHS 3, 2006) states that 20% of children under five in India are wasted,contributing to half of the global burden of malnutrition. SAMis responsible directly or indirectly for 35% of deaths among children under five years.
Objective: The objective of this study was to assess the demographic and clinical profiles of patients with SAM, assess effectiveness of NRC with relation to short term outcome and to assess compliance with the program and weight gainat the end of 2 months.
Methods: A retrospective study was conductedin children with SAM aged less than 5 years in the NRC at GMERS Medical College Vadodara. The study assessed all children for recovery and mortality at end of inpatient stay and at end of program at 60 days. The short-term outcomes were compared to the SPHERE standards 2011. Period of study was from January 2017 to December 2017. Variables assessed weregender, age at presentation, socio- economic criteria, co-morbidities, anthropometric criteria, mean weight gain and compliance with follow up. Inclusion criteria used were anthropometric and clinical criteria used for classification of SAM.
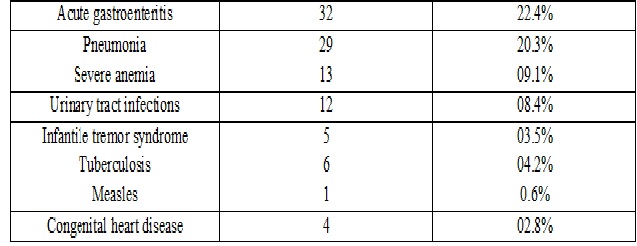
Results: 143 patients between age of 2 months to five years were admitted with SAM. The gender distribution for male to female patients was1.1:1. Majority of children were aged less than 2 years (78.3).89.5% childrenwere coming from families below poverty line and 38.5% were fully immunized for age.72.7% patients satisfied both anthropometric criteria. Commonest co- morbidity associated with SAM was diarrhea 22.4%, followed by lower respiratory tract infections 20.3%.Severe anemia was observed in 9.1% of patients. Outcomes were successful discharge in 93.7%, mortality in 2.1%, and default in 4.2%. 76.2% children showed weight gain at least 15% from baseline weight.Complete follow up (3 visits) was achieved in 57.3% patients.
Conclusion: Majority of patients presenting with SAM were belongingto below poverty line families which suggests that improving the socio economic conditions will have a positive impact on reduction on the incidence of severe malnutrition. Complete follow up visits were achieved in only half of the patients. Education of parents regarding the implications of malnutrition on long term quality of life and positive reinforcement for follow up can ensure that successfully discharged children do not default.
Downloads
References
2. National Family Health Survey (NHFS-4). Ministry of Health and Family Welfare.2015-2016.Availablefrom:URL: http://rchips.org/NFHS/pdf/NFHS4/India.pdf
3. WHO Guidelines Approved by the Guidelines Review Committee.Guideline: Updates on the Management of Severe Acute Malnutrition in Infants and Children. children.vol.2013.Geneva, 2013.p.6-54.
4. SPHERE: Sphere project: humanitarian charter and minimum standards in disaster response .2011.
5. Mission BalamSukham, Health and Family Welfare Department, Government of Gujarat. Available on www.gujhealth.gov.in/mission_balam_sukham.htm
6. Shewade HD, Sunderamurthy B, Jayakumar N, Ramadoss P. Prevalence of severe acute malnutrition (SAM) among under-five children: A community -based cross-sectional study from Puducherry India. Indian Journal of Maternal and Child Health. 2013;15(1):[8] p.
7. Shaza OH, Mohammed OS. Prevalence and outcome of severe malnutrition in children less than five -year -old in Omdurman Pediatric Hospital, Sudan.Sudanese Journal ofPaediatrics.2016;Vol 16(1):23-30.
8. Ubesei AC, Ibeziako NS, Ndiokwelu C, Uzoka CM, Nwafor CA. Under- five protein energy malnutrition admitted at the university of Nigeria Teaching Hospital, Enugu: a 10 year retrospective review. Nutrition Journal 2012;11:43-50.
9.Mathur A, Tahilramani G, Makhija S, Devgan V. Burden of Severe Acute Malnutrition in under-five Children (2-59 Months) Admitted in a Tertiary Care Hospital of Delhi. J Trop Pediatr. 2018 Feb 1;64(1):45-50. doi: 10.1093/tropej/fmx026 .[pubmed]
10. Nahar B, Ahmed T, Brown KH, Hossain MI. Risk Factors Associated with Severe Underweight among Young Children reporting to a Diarrhoea Treatment Facility in Bangladesh. Journal of Health Population and Nutrition October 2010; 28(5):476-483.
11. Mishra K, Kumar P, Basu S, Rai K, Aneja S. Risk factors for Severe Acute Malnutrition in children below five years of age in India: A case-control study. Indian Journal of Paediatrics. .2014 August;81(8):762-5.
12. Thapa A, Shah GS, Mishra OP. Analysis of Co-morbidities in Children with Severe Acute Malnutrition in Eastern Nepal. Journal of Nepal Paediatric Society 2015 May-August;35(2):9-102..
13. Saini DT, Verma DA, Berwal PK. Pattern of Co-morbidities in Children with Severe Acute Malnutrition admitted in MTC of a teaching hospital of Western Rajasthan, India. J Med Science and Clinical Research. 2016 April;4(4):10070-73.
Copyright (c) 2018 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


