A comparative Study of parenteral versus oral antibiotics in the treatment of severe pneumonia in children under five years of age
Abstract
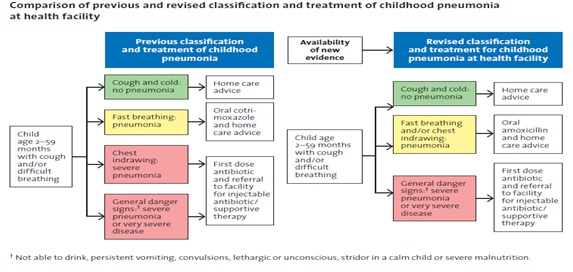
Introduction: Pneumonia is a disease known to mankind from antiquity. Pneumonia is an acute inflammation of the pulmonary parenchyma that can be caused by various infective and non-infective origins, presenting with physical and radiological features compatible with pulmonary consolidation of a part or parts of one or both lungs.
Objective: This study is aimed to compare parenteral versus oral antibiotics in the treatment of severe pneumonia in children under five years of age.
Materials and Methods: This is a prospective observational comparative study. This study was conducted in the department of pediatrics, MGM hospital, Kakatiya Medical College, Warangal. A total of 268 patients were recruited for the study as per the inclusion and exclusion criteria of the WHO guidelines for community acquired pneumonia.
Results: A total of 268 children have been enrolled in the present study. Treatment Failure rate in oral amoxicillin group is 12.6% and in Inj. ampicillin plus amikacin group is 11.1%. The difference in treatment outcome in the two treatment groups is NOT statistically significant. A total of 17 out of 134 children in oral amoxicillin group have progressed to treatment failure which amounts to a failure rate of 12.68%. More than half (7/15) of the children who progressed cumulatively to treatment failure in the inj ampicillin plus amikacin group have developed at least one of the signs of WHO defined very severe pneumonia.
Conclusion: In the present study it has been observed that there is no statistically significant difference in the failure rate in oral amoxicillin group and Inj. Ampicillin plus Inj. Amikacin group, suggesting similar outcome for severe pneumonia treated with oral amoxicillin and Inj. Ampicillin plus Amikacin.
Downloads
References
2. Bansal S, Kashyap S, Pal LS, Goel A. Clinical and bacteriological profile of community acquired pneumonia in Shimla, Himachal Pradesh. Indian J Chest Dis Allied Sci. 2004 Jan-Mar;46(1):17-22.[pubmed]
3. Díaz A, Barria P, Niederman M. et al.Etiology of community-acquired pneumonia in hospitalized patients in chile: the increasing prevalence of respiratory viruses among classic pathogens. Chest. 2007 Mar;131(3):779-787. doi: 10.1378/chest.06-1800.[pubmed]
4. Javed S, Chaudhry R, Passi K, et al. Sero diagnosis of Legionella infection in community acquired pneumonia. Indian J Med Res. 2010 Jan;131:92-6.[pubmed]
5. Shah BA, Singh G, Naik MA, Dhobi GN. Bacteriological and clinical profile of Community acquired pneumonia in hospitalized patients. Lung India. 2010 Apr;27(2):54-7. doi: 10.4103/0970-2113.63606.[pubmed]
6. Müller B, Harbarth S, Stolz D, et al. Diagnostic and prognostic accuracy of clinical and laboratory parameters in community-acquired pneumonia. BMC Infect Dis. 2007 Mar 2;7:10. DOI:10.1186/1471-2334-7-10
7. Metlay JP, Fine MJ. Testing strategies in the initial management of patients with community-acquired pneumonia. Ann Intern Med. 2003 Jan 21;138(2):109-18.[pubmed]
8. Kyriacou DN, Yarnold PR, Soltysik RC, et al. Derivation of a triage algorithm for chest radiography of community-acquired pneumonia patients in the emergency department. AcadEmerg Med. 2008 Jan;15(1):40-4. doi: 10.1111/j.1553-2712.2007.00011.x.[pubmed]
9. Metlay JP, Schulz R, Li YH, et al. Influence of age on symptoms at presentation in patients with community-acquired pneumonia. Arch Intern Med. 1997 Jul 14;157(13):1453-9.[pubmed]
10. Leowski J. Mortality from acute respiratory infections in children under 5 years of age: Global estimates. World Health Statistics Quarterly. 1986; 39:138–44.
11. Levels and Trends in Child Mortality: Report 2014. United Nations Inter Agency Group for Child Mortality Estimation UNICEF, WHO, TheWorld Bank, United Nations Population Division. New York, 2014.
12. Global Health Observatory. Proportions of child deaths by cause. WHO, Geneva.
13. Walker CLF, Rudan I, Liu L, et al. Global burden of childhood pneumonia and diarrhoea. Lancet. 2013 Apr 20;381(9875):1405-1416. doi: 10.1016/S0140-6736(13)60222-6. Epub 2013 Apr 12.[pubmed]
14. Shann F. Etiology of severe pneumonia in children in developing countries. Pediatr Infect Dis. 1986 Mar-Apr;5(2):247-52.[pubmed]
15. Cherian T. Acute respiratory infections in developing countries: current status and future directions. Indian Pediatr1997; 34: 877-884.[pubmed]
16. WHO. Programme for control of acute respiratory infections. Acute respiratory infections in children: case management in Small hospitals in developing countries - A Manual for Doctors and Senior Health Workers. Geneva WHO/ARI/90.5.
17. Integrated Management of Childhood Illness (IMCI). Geneva, World Health Organization/The United Nation Children’s Fund (UNICEF), 2008.
18. Integrated Management of Childhood Illness (IMCI). WHO recommendations on the management of diarrhoea and pneumonia in HIV-infected infants and children. Geneva: 2010.
19. Sazawal S, Black RE; Pneumonia Case Management Trials Group. Effect of pneumonia case management on mortality in neonates, infants, and preschool children: a meta-analysis of community-based trials. Lancet Infect Dis. 2003 Sep;3(9):547-56.[pubmed]
20. RudanI, Pinto CB,Biloglav Z, Mulholland K, Campbell H. Epidemiology and etiology of childhood pneumonia. Bulletin of the World Health Organization. 2008; 86:408–416.
21. Bang AT, Bang RA, Reddy HM. Home-based neonatal care: summary and applications of the field trial in rural Gadchiroli, India (1993 to 2003). J Perinatol. 2005 Mar;25 Suppl1:S108-22.[pubmed]
22. The Multi-Country Evaluation of IMCI Effectiveness, Cost and Impact (MCE) – Progress Report’, May 2001–April 2002, Geneva: World Health Organization; 2002 (WHO/FCH/CAG/02.16).
23. Aguilar AM et al. Mortality Survey of Bolivia: The Final Report: Investigating and identifying the causes of death for children under five. Published for USAID by the Basic Support for Institutionalizing Child Survival (BASICS) Project, Virginia, 1998.
24. Schumacher R et al. Mortality Study in Guinea: Investigating the causes of death in children under 5. Published by Save the Children and the Basic Support for Institutionalizing Child Survival (BASICS II) Project, Virginia, 2002.
25. Schellenberg JA, Victora CG, Mushi A, et al. Inequities among the very poor: health care for children in rural southern Tanzania. Lancet. 2003 Feb 15;361(9357):561-6. DOI:10.1016/S0140-6736(03)12515-9
26. World Health Organization. Recommendations for management of common childhood conditions: evidence for technical update of pocket book recommendations: newborn conditions, dysentery, pneumonia, oxygen use and delivery, common causes of fever, severe acute malnutrition and supportive care. Geneva, Switzerland: WHO, 2012.
27. Addo-Yobo E, Chisaka N, Hassan M, Hibberd P, Lozano JM, Jeena B. Oral amoxicillin versus injectable penicillin for severe pneumonia in children aged 3to 59 months: a randomisedmulticentre equivalency study. Lancet 2004; 364 (9440): 1141–8.
28. Ambrose Agweyu, Davis Gathara, Jacquie Oliwa, Naomi Muinga, Tansy Edwards, Elizabeth Alen, et al. Oral Amoxicillin Versus Benzyl Penicillin for Severe Pneumonia Among Kenyan Children. A Pragmatic Randomized Controlled Noninferiority Trial. Clinical Infectious Diseases, 2015; 60 (8): 1216–1224.
29. Hazir T, Fox LM, Bin Nisar YB, Fox MP, Ashraf YP, et al. Ambulatory short-course high-dose oral amoxicillin for treatment of severe pneumonia in children: a randomised equivalency trial. Lancet 2008; 371 (9606): 49–56.
30. Atkinson M, Lakhanpaul M, Smyth A, Vyas H, Weston V, et al. Comparison of oral amoxicillin and intravenous benzyl penicillin for community acquired pneumonia in children (PIVOT trial): a multicentre pragmatic randomised controlled equivalence trial. Thorax 62 (12): 1102–1106.
31. Addo-Yobo E, Anh DD, El-Sayed HF, Fox LM, Fox MP, et al. Outpatient treatment of children with severe pneumonia with oral amoxicillin in four countries: the MASS study. Trop Med Int Health 2011; 16 (8): 995–1006.[pubmed]
32. Addo-Yobo E, Anh DD, El-Sayed HF, et al. Outpatient treatment of children with severe pneumonia with oral amoxicillin in four countries: the MASS study. Trop Med Int Health. 2011 Aug;16(8):995-1006. doi: 10.1111/j.1365-3156.2011.02787.x.Epub 2011 May 4.[pubmed]
Copyright (c) 2018 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


