Study on clinical profile and etiology of acute febrile encephalopathy in children aged between 2 months to 14 years attending to a tertiary care hospital, Eluru, Andhra Pradesh, India
Abstract
Background: Acute febrile encephalopathy (AFE) is a common conditionleading to hospitalization of children in India. CNS infections are commonest cause of non-traumatic coma in children. Although AFE is one of the major causes of hospital admissions of children and adults in India, only a few studies have been done on it so far.So this study was conducted to study the clinical profile and etiology of AFE in children.
Methods: This prospective study was carried out on 84 children between 2 months to 14 years, with fever duration of<14 days, GCS ≤12 at the time of admission and altered sensorium in the pediatric intensive care unit over a period of 12 months from August 2017 to August 2018. Clinical profile and etiology were evaluated.
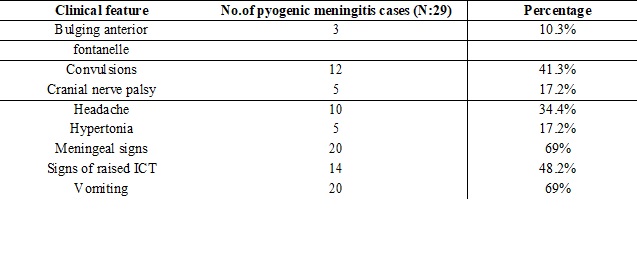
Results: Thepresent study, has identified viral encephalitis (38%) and pyogenic meningitis (34.5%) as the major causes of Acute febrile encephalopathy in the study population. Most common symptoms apart from fever and altered sensorium were vomiting (58.3%), convulsions (45.2%), headache (35.7%), jaundice (8.3%), and most common presenting clinical signs apart from fever and GCS< 12 were neck stiffness (52.4%), signs of raised ICT (47.6%), positive Kernig’s sign (39.2%), and motor tone abnormalities (34.5%).
Conclusion: In this study, we observed that CNS infections are the most common cause of febrile encephalopathy in children. Early recognition of the clinical signs and immediate and appropriate treatment will combat the problem and improve the survival rate.
Downloads
References
2. Abend NS, Licht DJ. Predicting outcome in children with hypoxic ischemic encephalopathy. PediatrCrit Care Med. 2008 Jan;9(1):32-9. doi: 10.1097/01.PCC.0000288714.61037.56.[pubmed]
3. Bansal A, Singhi SC, Singhi PD, Khandelwal N, Ramesh S. Nontraumatic coma. Indian J Pediatr. 2005;72(6):467-73.[pubmed]
4. Bhalla A, Suri V, Varma S, et al. Acute febrile encephalopathy in adults from Northwest India. J Emerg Trauma Shock. 2010 Jul;3(3):220-4. doi: 10.4103/0974-2700.66520.
5. Duke T, Riddell M, Barnabas R. The aetiology, clinical presentations and outcome of febrile encephalopathy in children. Annal Trop Paediatr: Int Child Health. 2010;30:109-18.
6. Singh RR, Chaudhary SK, Bhatta NK, et al.Clinical and etiological profile of acute febrile encephalopathy in eastern Nepal. Indian J Pediatr. 2009 Nov;76(11):1109-11. doi: 10.1007/s12098-009-0233-8.[pubmed]
7. Kothari VM1, Karnad DR, Bichile LS. Tropical infections in the ICU. J Assoc Physicians India. 2006 Apr;54:291-8.[pubmed]
8. Rupa. R Singh, S.K.Chaudhary, Nisha K. Bhatta, B. Khanal and Dheeraj Shah. Clinical and etiological profile of acute febrile encephalopathy in Eastern Nepal; Indian Journal of Pediatrics 2009:76(11):1109-1111.
9. S.A Karmarkar, Satinder Aneja, ShasiKhare, Arun Saini, Anju Seth and B. K. Y. Chauhan. A study of Acute febrile encephalopathy with special reference to viral etiology. Indian journal of pediatrics 2008,volume 75(8):801-805.[pubmed]
10. Anga G, Barnabas R, Kaminiel O, tefuarani N, Vince J, Ripa P, Riddell M,DukeT.Theaetiology,clinical presentations and outcome of febrile encephalopathy in children in Papua New Guinea; Ann Trop Pediatr :2010;30(2):109-18.
11. Verma S, Ramachandran VG. Acute encephalopathy in Western Uttar Pradesh. Indian Pediatr. 2007 Apr;44(4):310.[pubmed]
12. Elsaid MF, Flamerzi AA, Bessisso MS, Elshafie SS. Acute bacterial meningitis in Qatar. Saudi Med J. 2006 Feb;27(2):198-204.[pubmed]
13. S.Curtis et al. Clinical features suggestive of meningitis in children. A systemic review of prospective data. Pediatrics, official J of American Academy of Pediatrics; 2010;126(5) :952-960.
14. Sushant S Mane et al. Changing trends in clinical presentation of Paediatric cerebral malaria. Dec 2012;vol 9:issue 12.doi 10.7199/ped.on call 2012.80
15. G.S. Tanwar et al. Clinical profile of 13 children with P. vivax cerebral malaria. Annals of Tropical paediatrics 2011:31(4) :351-356.
16. Thilothammal et al. Tuberculous meningitis in children, mortality and morbidity of bacteriologically confirmed cases; Indian pediatric neurology, 1995 June;32(6):641-647.
Copyright (c) 2018 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


