High flow nasal cannula vs non-invasive ventilation in pediatric ARDS: an RCT
Abstract
Introduction: Pediatric Acute Respiratory Distress syndrome (PARDS) has been re-defined (2015) as per the final recommendations of the Pediatric Acute Lung Injury Consensus Conference. The use of high flow nasal cannula is a promising treatment but its efficacy compared with non invasive ventilation (NIV) is not known.
Aims and Objectives: The current study was undertaken to study the efficacy of high flow nasal cannula compared with NIV in PARDS.
Methods: This was a pilot randomized controlled trial done in the PICU of a tertiary care teaching hospital over 10 months (December 2017 – September 2018). All patients aged 1-18 years of age, who presented with or developed ARDS during their course of hospitalization, and who fulfilled the inclusion criteria, were randomized to receive HFNC and Continuous Positive Airway Pressure (NIV) as the initial respiratory support.Details were noted in a pre-designed standardized data collection form, entered into MS-EXCEL worksheet 2013 and analyzed using the Epi info software version 7.2.0.1.
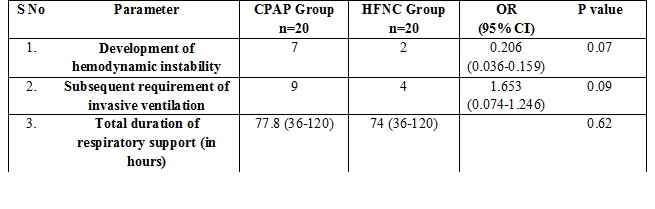
Results: A total of 40 patients were enrolled, 20 in each arm.Of these majority (25/40=62.5%) were boys. Majority of these patients were from rural or semi-urban areas (28/40=70.0%) and belonged to low socio-economic class (33/40= 82.5%) patients.Underlying diagnosis was sepsis in the majority (27/40=67.5%) patients.Twenty one (23/40=57.5%) patients had co-existent pneumonia.Development of hemodynamic instability approached statistical significance in being low in HFNC group compared with the CPAP group (p=0.07; OR 0.206, 95% CI 0.036-0.159).Subsequent requirement of invasive ventilation was also low in HFNC group compared with CPAP group and approached significance (p=0.09; OR 1.653, 95% CI 0.074-1.246). Total duration of respiratory support (p=0.62) was comparable in both the groups.
Conclusion: HFNC is efficacious in managing PARDS. Subsequent requirement of invasive ventilation and hemodynamic deterioration was significantly low with HFNC compared with NIV (CPAP).
Downloads
References
2. Pediatric Acute Lung Injury Consensus Conference Group. Pediatric acute respiratory distress syndrome: consensus recommendations from the Pediatric Acute Lung Injury Consensus Conference. PediatrCrit Care Med. 2015 Jun;16(5):428-39. doi: 10.1097/PCC.0000000000000350.[pubmed]
3. Gupta S, Sankar J, Lodha R, et al. Comparison of Prevalence and Outcomes of Pediatric Acute Respiratory Distress Syndrome Using Pediatric Acute Lung Injury Consensus Conference Criteria and Berlin Definition. Front Pediatr. 2018 Apr 9;6:93. doi: 10.3389/fped.2018.00093. eCollection 2018.[pubmed]
4. Grassi A, Foti G, Laffey JG, et al. Noninvasive mechanical ventilation in early acute respiratory distress syndrome. Pol Arch Intern Med. 2017 Sep 29;127(9):614-620. doi: 10.20452/pamw.4088. Epub 2017 Aug 17.
5. Wolfler A, Raimondi G, Pagan de Paganis C, Zoia E. The infant with severe bronchiolitis: from HFNC to CPAP and mechanical ventilation. Minerva Pediatr. 2018 Oct 18. doi: 10.23736/S0026-4946.18.05358-6. [Epub ahead of print]
6. Randolph AG. Management of acute lung injury and acute respiratory distress syndrome in children. Crit Care Med. 2009 Aug;37(8):2448-54. doi: 10.1097/CCM.0b013e3181aee5dd.[pubmed]
7. Messika J, Ben Ahmed K, Gaudry S, et al. Use of High-Flow Nasal Cannula Oxygen Therapy in Subjects With ARDS: A 1-Year Observational Study. Respir Care. 2015 Feb;60(2):162-9. doi: 10.4187/respcare.03423. Epub 2014 Nov 4.[pubmed]
8. Kumar SS, SelvarajanChettiar KP, Nambiar R. et al. Etiology and Outcomes of ARDS in a Resource Limited Urban Tropical Setting. J Natl Med Assoc. 2018 Aug;110(4):352-357. doi: 10.1016/j.jnma.2017.07.002. Epub 2017 Jul 18.[pubmed]
9. Luo Y, Ou R, Ling Y, et al. [The therapeutic effect of high flow nasal cannula oxygen therapy for the first imported case of Middle East respiratory syndrome to China]. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2015 Oct;27(10):841-4.[pubmed]
10. Frat JP, Brugiere B, Ragot S, et al. Sequential application of oxygen therapy via high-flow nasal cannula and noninvasive ventilation in acute respiratory failure: an observational pilot study. Respir Care. 2015 Feb;60(2):170-8. doi: 10.4187/respcare.03075. Epub 2014 Oct 7.[pubmed]
11.Vito Fanelli, AikateriniVlachou, Shirin Ghannadian, Umberto Simonetti, Arthur S. Slutsky, and Haibo Zhang. Acute respiratory distress syndrome: new definition, current and future therapeutic options. J Thorac Dis. 2013 Jun; 5(3): 326–334. doi: [10.3978/j.issn.2072-1439.2013.04.05]
12. Westhoff M, Schönhofer B, Neumann P, et al. Noninvasive Mechanical Ventilation in Acute Respiratory Failure. Pneumologie. 2015 Dec;69(12):719-756. doi: 10.1055/s-0034-1393309. Epub 2015 Dec 9.DOI:
Copyright (c) 2018 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


