Current Scenario of Neonatal Sepsis in West U.P
Abstract
Background: Sepsis is a significant cause of morbidity and mortality in neonates. Babies born with weight which is ≤2500 grams and those who are born prematurely are the main victims of neonatal sepsis. Early and prompt diagnosis is very crucial for intact survival. Clinical symptoms alone cannot be taken as a criteria to diagnose neonatal sepsis. Thus, for early diagnosis of neonatal sepsis, in addition to clinical signs and symptoms, a test is required which is easy, affordable and rapid.
Materials and Method: A cross sectional study was done between March, 2017 and May, 2018 in the Department of Pediatrics, S.N. Medical College, Agra. Before giving the first shot of antibiotic, blood samples of neonates were obtained by peripheral venous puncture under strict aseptic precautions and were evaluated for serial C- Reactive protein levels and complete blood counts. Blood culture were sent in all suspected sepsis neonates.
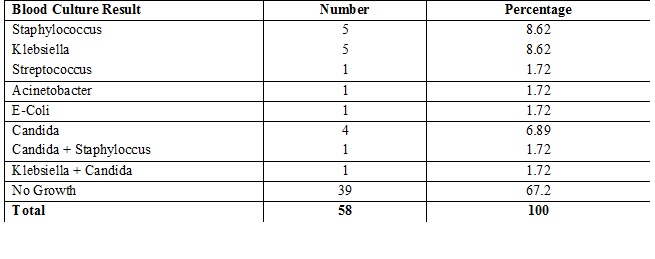
Results: Among total 58 suspected sepsis cases, 22 and 36 were females and males respectively; 8 neonates were Extremely Low Birth Weight, 14 were Very Low Birth Weight, 17 were Low Birth Weight & 19 were of normal birth weight; 38 and 20 neonates were preterm and term respectively; 21 presented within 72 hours of birth while 37 neonates were of Late onset sepsis. C-Reactive Protein were positive in 70.6% cases initially and 86.2% cases were positive after 24 hours. 19 were found to be proven culture positive.
Conclusion: Serial C-Reactive Protein measurement is a better indicator of neonatal sepsis. In addition to clinical signs and symptoms and presence of neonatal and maternal risk factors, serial C-Reactive Protein should be used to detect early and late neonatal sepsis. Probable sepsis cases should always be confirmed with blood culture.
Downloads
References
2. Schuchat A. Neonatal group B streptococcal disease--screening and prevention. N Engl J Med. 2000 Jul 20;343(3):209-10. DOI:10.1056/NEJM200007203430310.[pubmed]
3. Hornik CP, Fort P, Clark RH, et al. Early and late onset sepsis in very-low-birth-weight infants from a large group of neonatal intensive care units. Early Hum Dev. 2012 May;88 Suppl 2:S69-74. doi: 10.1016/S0378-3782(12)70019-1.[pubmed]
4. Edwards MS, Gonik B. Preventing the broad spectrum of perinatal morbidity and mortality through group B streptococcal vaccination. Vaccine. 2013 Aug 28;31 Suppl 4:D66-71. doi: 10.1016/j.vaccine.2012.11.046. Epub 2012 Nov 28.[pubmed]
5. Franciosi RA, Knostman JD, Zimmerman RA. Group B streptococcal neonatal and infant infections. J Pediatr. 1973 Apr;82(4):707-18.[pubmed]
6. Bauserman MS, Laughon MM, Hornik CP, et al. Group B Streptococcus and Escherichia coli infections in the intensive care nursery in the era of intrapartum antibiotic prophylaxis. Pediatr Infect Dis J. 2013 Mar;32(3):208-12. doi: 10.1097/INF.0b013e318275058a.[pubmed]
7. Guilbert J, Levy C, Cohen R; et al. Late and ultra late onset Streptococcus B meningitis: clinical and bacteriological data over 6 years in France. Acta Paediatr. 2010 Jan;99(1):47-51. doi: 10.1111/j.1651-2227.2009.01510.x.[pubmed]
8. Lin TY, Kao HT, Hsieh SH, et al. Neonatal enterovirus infections: emphasis on risk factors of severe and fatal infections. Pediatr Infect Dis J. 2003 Oct;22(10):889-94. DOI:10.1097/01.inf.0000091294.63706.f3
9. Stoll BJ, Hansen N, Fanaroff AA, et al. Changes in pathogens causing early-onset sepsis in very-low-birth-weight infants. N Engl J Med. 2002 Jul 25;347(4):240-7. DOI:10.1056/NEJMoa012657.[pubmed]
10. Hoffman JA, Mason EO, Schutze GE, et al. Streptococcus pneumoniae infections in the neonate. Pediatrics. 2003 Nov;112(5):1095-102.[pubmed]
11. Bizzarro MJ, Raskind C, Baltimore RS, et al. Seventy-five years of neonatal sepsis at Yale: 1928-2003. Pediatrics. 2005 Sep;116(3):595-602. DOI:10.1542/peds.2005-0552.[pubmed]
12. Stoll BJ, Gordon T, Korones SB, et al. Late-onset sepsis in very low birth weight neonates: a report from the National Institute of Child Health and Human Development Neonatal Research Network. J Pediatr. 1996 Jul;129(1):63-71.[pubmed]
13. Lim WH, Lien R, Huang YC, et al. Prevalence and pathogen distribution of neonatal sepsis among very-low-birth-weight infants. Pediatr Neonatol. 2012 Aug;53(4):228-34. doi: 10.1016/j.pedneo.2012.06.003. Epub 2012 Jul 23.[pubmed]
14. Mussap M, Noto A, Cibecchini F, et al. The importance of biomarkers in neonatology. Semin Fetal Neonatal Med. 2013 Feb;18(1):56-64. doi: 10.1016/j.siny.2012.10.006. Epub 2012 Nov 17.[pubmed]
15. Aggarwal R, Sarkar N, Deorari AK, et al. Sepsis in the newborn. Indian J Pediatr. 2001 Dec;68(12):1143-7.[pubmed]
16. Chacko B, Sohi I. Early onset neonatal sepsis. Indian J Pediatr. 2005 Jan;72(1):23-6.[pubmed]
17. Tallur SS, Kasturi AV, Nadgir SD, et al. Clinico-bacteriological study of neonatal septicemia in Hubli. Indian J Pediatr. 2000 Mar;67(3):169-74.[pubmed]
18. Raghavan M, Mondal GP, Bhat BV, et al. Perinatal risk factors in neonatal infections. Indian J Pediatr. 1992 May-Jun;59(3):335-40.[pubmed]
19. Chiesa C, Panero A, Osborn JF, et al. Diagnosis of neonatal sepsis: a clinical and laboratory challenge. Clin Chem. 2004 Feb;50(2):279-87. DOI:10.1373/clinchem.2003.025171.[pubmed]
20. Schelonka RL, Chai MK, Yoder BA, et al. Volume of blood required to detect common neonatal pathogens. J Pediatr. 1996 Aug;129(2):275-8.[pubmed]
21. Karthikeyan G, Premkumar K. Neonatal sepsis: Staphylococcus aureus as the predominant pathogen. Indian J Pediatr. 2001 Aug;68(8):715-7.[pubmed]
22. Kumhar GD, Ramachandran VG, Gupta P. Bacteriological analysis of blood culture isolates from neonates in a tertiary care hospital in India. J Health Popul Nutr. 2002 Dec;20(4):343-7.[pubmed]
23. Rani R, Mohapatra NP, Mehta G, Randhawa VS. Changing trends of Candida species in neonatal septicemia in a tertiary north Indian hospital. Indian J Med Microbiol. 2002; 20(1):42–4.
24. Benitz WE, Han MY, Madan A, et al. Serial serum C-reactive protein levels in the diagnosis of neonatal infection. Pediatrics. 1998 Oct;102(4):E41.[pubmed]
25. Hisamuddin E, Hisam A, Wahid S, et al. Validity of C-reactive protein (CRP) for diagnosis of neonatal sepsis. Pak J Med Sci. 2015;31(3):527-31. doi: 10.12669/pjms.313.6668.[pubmed]
26. Hofer N, Zacharias E, Müller W, et al. An update on the use of C-reactive protein in early-onset neonatal sepsis: current insights and new tasks. Neonatology. 2012;102(1):25-36. doi: 10.1159/000336629. Epub 2012 Apr 11.[pubmed]
Copyright (c) 2018 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


