Effect of surfactant in respiratory distress syndrome as early rescue therapy verses delayed selective therapy in 28 to 32 weeks of gestation
Abstract
Background: This prospective interventional study is designed to compare effect of giving surfactant in Respiratory Distress Syndrome (RDS), stabilized on CPAP, as Early Rescue Therapy verses Delayed Selective therapy in Early Pre-terms 28 to 32 weeks, using INSURE method. The main objectives if the studies are to study survival rate and mortality rate in the two groups and to compare the various complications of RDS and surfactant therapy in two groups.
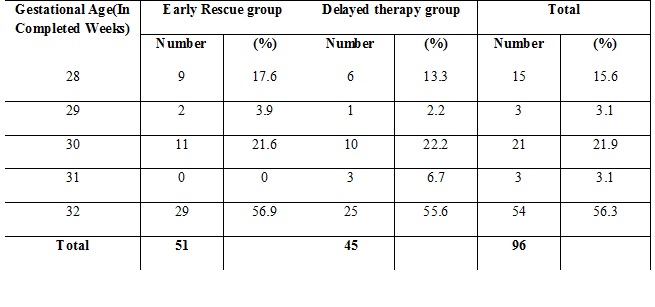
Methods: Cases were selected from the Preterm newborn, 28-30 weeks of gestation, confirmed cases of RDS on the basis of Chest X-ray findings and shake test, admitted. Total 96 cases were enrolled, out of which 51 randomly allotted to Early Rescue therapy and 45 to Delayed Selective treatment. Surfactants were administered using INSURE technique. Observations, clinical findings, course of treatment, vitals and outcomes were noted. Data was analyzed using appropriate statistical methods. Efforts were made to study maximum parameters to find out, which treatment strategy provides better outcomes and feasible in our settings.
Results: In Early group more cases (68.6%) are discharged than in Delayed group (66.7%). Survival rate is more in Early group. In Early group less mortality is seen 16(31.4%), than in Delayed group 15(33.3%). Mean total duration of stay in NICU is decreased in Early group (7.08±6.209 days) as compared to Delayed group (8.896.±793 days).
Conclusion: Early Rescue Therapy increases the survival rate of preterm than the Delayed selective Treatment. Survival rate is increased when surfactant is administered earlier, less than two hours of life, during the course of RDS. Mortality is reduced in Early administration of surfactant but pulmonary causes of mortality is more in them as compared to Delayed administration, where pulmonary as well as non-pulmonary causes of death both affect the mortality.
Downloads
References
2. Kendig JW, Ryan RM, Sinkin RA, Maniscalco WM, Notter RH, Guillet C, et al. Comparison of two strategies for surfactant prophylaxis in very premature infants: a multicenter randomized trial. Pediatrics.1998;101:100612.
3. Velaphi S. Early versus delayed selective surfactant treatment for neonatal respiratory distress syndrome: RHL commentary (last revised: 1 September 2010). The WHO Reproductive Health Library; Geneva: World Health Organization.[pubmed]
4. European Exosurf Study; Early or selective surfactant (colfosceril palmitate, Exosurf) for intubated babies at 26 to 29 weeks gestation. A European double-blind trial with sequential analysis..Online J Curr Clin Trials. 1992 Nov 10; Doc No 28:[3886 words; 47 paragraphs].[pubmed]
5. Femitha P, Rojo Joy, Adhisivam B, Bahubali D Gane, Vishnu Bhat B, Surfactant Replacement Therapy(SRT) in Respiratory Distress Syndrome(RDS), Curr Pedistr Res 2012; 16(2):134-136
6. Halliday HL. Natural vs. synthetic surfactants in neonatal respiratory distress syndrome. Drugs. 1996;51:226-37.[pubmed]
7. Sandri F, Plavka R, Ancora G, Simeoni U, Stranak Z, Martinelli S, et al. CURPAP Study Group. Prophylactic or early selective surfactant combined with nCPAP in very preterm infants. Pediatrics. 2010;125:e1402-9.[pubmed]
8. Konishi M1, Fujiwara T, Chida S, Maeta H, Shimada S, Kasai T, Fujii Y, Murakami Y. A prospective, randomized trial of early versus late administration of a single dose of surfactant-TA. Early Hum Dev. 1992 Jun-Jul;29(1-3):275-82.
9. Gortner L1, Wauer RR; Early versus late surfactant treatment in preterm infants of 27 to 32 weeks' gestational age: a multicenter controlled clinical trial.Pediatrics. 1998 Nov;102(5):1153-60. [pubmed]
10. Early versus delayed neonatal administration of a synthetic surfactant--the judgment of OSIRIS. The OSIRIS Collaborative Group (open study of infants at high risk of or with respiratory insufficiency--the role of surfactant.Lancet. 1992 Dec 5;340(8832):1363-9.[pubmed]
11. SUPPORT Study Group of the Eunice Kennedy Shriver NICHD Neonatal Research Network, Finer NN, Carlo WA, Walsh MC, Rich W, Gantz MG, et al. Early CPAP versus surfactant in extremely preterm infants. N Engl JMed 2010;362:1970e9.[pubmed]
12. Aguar M, Cernada M, Brugada M, Gimeno A, Gutierrez A, Vento M. Minimally invasive surfactant therapy with a gastric tube is as effective as the intubation, surfactant, and extubation technique in preterm babies. ActaPaediatr. 2014;103:e229-33.[pubmed]
13. More K, Sakhuja P, Shah PS. Minimally invasive surfactant administration in preterm infants: A meta-narrative review. JAMA Pediatr.2014;168:901-8.[pubmed]
14. Gregory GA, Kitterman JA, Phibbs RH, Tooley W, Hamilton WK. Treatment of idiopathic respiratory distress syndrome with continuous positive airway pressure. N Engl J Med 1971; 284: 1333-1340.[pubmed]
15. Lee US, Dunn MS, Fenwick M, Shennan AT. A comparison of underwater bubble continuous positive airway pressure (CPAP) with ventilator derived CPAP in preterm neonates ready for extubation. Biol Neonate 1998; 73: 69-75.[pubmed]
16. More K, Sakhuja P, Shah PS. Minimally invasive surfactant administration in preterm infants: A meta-narrative review. JAMA Pediatr.2014;168:901-8.[pubmed]
17. Gregory GA, Kitterman JA, Phibbs RH, Tooley W, Hamilton WK. Treatment of idiopathic respiratory distress syndrome with continuous positive airway pressure. N Engl J Med 1971; 284: 1333-1340.[pubmed]
18. Lee US, Dunn MS, Fenwick M, Shennan AT. A comparison of underwater bubble continuous positive airway pressure (CPAP) with ventilator derived CPAP in preterm neonates ready for extubation. Biol Neonate 1998; 73: 69-75.[pubmed]
19. Klerk AMD, Klerk RKD. Nasal CPAP and outcomes of pre term infants. J Pediatr Child Health 2001; 37: 161-167.[pubmed]
20. Early versus delayed neonatal administration of a synthetic surfactant--the judgment of OSIRIS. The OSIRIS Collaborative Group (open study of infants at high risk of or with respiratory insufficiency--the role of surfactant.Lancet. 1992 Dec 5;340(8832):1363-9.[pubmed]
21. Victor Yu, Professor of Neona- tology, Monash University, Director of Neonatal Intensive Care, Monash Medical Center, Australia. Surfactant Replacement Therapy Review Article Indian Pediatrics 1998; 35:1081-1096.
22. Evans J J. Prediction of respiratory distress syndrome by shake test on newborn gastric aspirate. N Engl J Medicine 1975; 292: 1113-1115.[pubmed]
23. Arya LS, Singh M. Gastric shake test as predictor of hyaline membrane disease. Indian J Med Res 1979; 70: 444-48.[pubmed]
Copyright (c) 2018 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


