Profile of Anemia with special reference to hemoglobinopathies in a tertiary care centre in Madhya Pradesh
Abstract
Introduction: Haemoglobinopathies constitute very important causative factors for anemia of childhood, especially in those regions where abnormal hemoglobin genes are highly prevalent. Thalassemia and Sickle cell anemia can be prevented by proper genetic counseling and screening.
Material Methods: This cross-sectional one year study was conducted at Sri Aurobindo hospital Indore in department of pediatrics with the primary objective is to find out clinical and hematological characteristics of anemia with special reference to hemoglobinopathy. A total of 100 subjects were included.
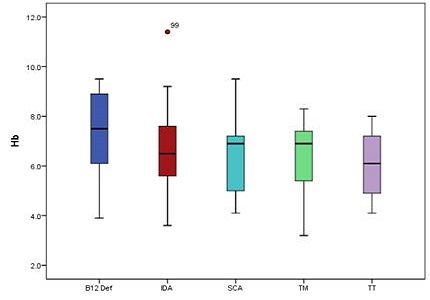
Results: The mean age of patients was 4.63 ± 4.18 years. Prevalence of Iron deficiency anemia was 61%, Vitamin B12 deficiency was 12%, thalassemia trait 10%, sickle cell anemia 10% and thalassemia major was 7%. , Mean Hb concentration was 6.54±1.63 g/dl and the MCV values ranged between 59.2±5.8 and 100.7±13.9. Mean reticulocyte was found 3.85±2.11 in thalassemia major, 4.0±2.10 and4.6±2.5 in sickle cell anemia. Mean HbA2 level was 2.45±0.69, in thalassemia major, 5.13±0.61 in thalassemia trait, and 2.01±0.71 in sickle homozygous. Mean HbF level was 92.57±1.6 in thalassemia major, 2.15±1.24 in thalassemia trait and 20.2± 9.6 in sickle cell anemia.
Conclusion: HPLC is a reliable method for screening of thalassemia.Screening should be done among all suspected patients to find out the exact prevalence of thalassemia. Treatment should be started as soon as thalassemia positive is detected before the end organ damage has occurred. Genetic counseling of the patient’s family for next pregnancy should be done to avoid birth of a thalassemia child in their family.
Downloads
References
2. Jain S, Chopra H, Garg SK, Bhatnagar M, Singh JV. Anemia in children: early iron supplementation. Indian J Pediatr. 2000 Jan;67(1):19-21. [PubMed]
3. Rasmussen Z, Pio A, Enarson P. Case management of childhood pneumonia in developing countries: recent relevant research and current initiatives. Int J Tuberc Lung Dis. 2000 Sep;4(9):807-26. [PubMed]
4. Muwakkit S, Nuwayhid I, Nabulsi M, al Hajj R, Khoury R, Mikati M, Abboud MR. Iron deficiency in young Lebanese children: association with elevated blood lead levels. J Pediatr Hematol Oncol. 2008 May;30(5):382-6. doi: 10.1097/MPH.0b013e318165b283. [PubMed]
5. Martin PL, Pearson HA. The anemias. In: Oski FA. Principles and practices of pediatrics. 2nd ed. Philadelphia: J. B. Lippincott, 1994.pp.1657-1658.
6. Nathan DG, Orkin SH, Oski FA, Ginsburg D. Nathan and Oski's Hematology of infancy and childhood. 5th ed. Philadelphia: Saunders, 1998:382.
7. Bessman JD, Gilmer PR Jr, Gardner FH. Improved classification of anemias by MCV and RDW. Am J Clin Pathol. 1983 Sep;80(3):322-6. [PubMed]
8. Weatherall DJ, Clegg JB. Thalassemia syndrome 4th edition. Blackwell Science Oxford, 2001 [PubMed]
9. Martin A, Thompson AA. Thalassemias. Pediatr Clin North Am. 2013 Dec;60(6):1383-91. doi: 10.1016/j.pcl.2013.08.008. Epub 2013 Oct 4. [PubMed]
10. Galanello R, Origa R. Beta-thalassemia. Orphanet J Rare Dis. 2010 May 21;5:11. doi: 10.1186/1750-1172-5-11. [PubMed]
11. Sarnaik SA. Thalassemia and related hemoglobinopathies. Indian J Pediatr. 2005 Apr;72(4):319-24. [PubMed]
12. WHO-Executive Board EB118/5, 118th Session Report by the Secretariat on thalassemia and other hemoglobinopathies: Prevalence of hemoglobinopathies. 11 May 2006. p. 1-8.
13. Mohanty D, Colah RB, Gorakshakar AC, Patel RZ, Master DC, Mahanta J, Sharma SK, Chaudhari U, Ghosh M, Das S, Britt RP, Singh S, Ross C, Jagannathan L, Kaul R, Shukla DK, Muthuswamy V. Prevalence of β-thalassemia and other haemoglobinopathies in six cities in India: a multicentre study. J Community Genet. 2013 Jan;4(1):33-42. doi: 10.1007/s12687-012-0114-0. Epub 2012 Oct 21.
14. Madan N, Sharma S, Sood SK, Colah R, Bhatia LH. Frequency of β-thalassemia trait and other hemoglobinopathies in northern and western India. Indian J Hum Genet. 2010 Jan;16(1):16-25. doi: 10.4103/0971-6866.64941. [PubMed]
15. Balgir RS. Genetic heterogeneity of population structure in 15 major scheduled tribes in central and eastern India: A study of immuno-hematological disorders. Indian J Hum Genet 2006;12:86-92. DOI: 10.4103/0971-6866.27792
16. Sukumaran PK. Abnormal hemoglobins in India. In: Sen NN, Basu AK, editors. Trends in Hematology. Calcutta: Saraswati Press; 1975. p. 225-36.
17. Balgir RS. Spectrum of hemoglobinopathies in the state of Orissa, India: a ten years cohort study. J Assoc Physicians India. 2005 Dec;53:1021-6. [PubMed]
18. Verma IC, Choudhry VP, Jain PK. Prevention of thalassemia: a necessity in India. Indian J Pediatr. 1992 Nov-Dec;59(6):649-54. [PubMed]
19. Manglani M, Lokeshwar MR, Vani VG, Bhatia N, Mhaskar V. 'NESTROFT'--an effective screening test for beta thalassemia trait. Indian Pediatr. 1997 Aug;34(8):702-7.
20. Wild BJ, Bain BJ. Investigation of abnormal hemoglobins and thalassemia. In: Lewis SM, Bain BJ, Bates I (Eds.), Dacie and Lewis Practical Hematology, 9th Edition. London : Churchill Livingstone. 2001; 231-268.
21. World Health Organization. Measuring change in nutritional Status. Guidelines for assessing impact of supplementary feeding programmes for vulnerable groups. World Health Organization: Geneva. 1983. Available from: https://extranet.who.int/iris/restricted/bitstream/10665/38768/1/9241541660.pdf
22. Saba F, Poornima S, Balaji PAR, Varne SRR, Jayashree K. Anemia Among Hospitalized Children at a Multispecialty Hospital, Bangalore (Karnataka), India. Journal of Family Medicine and Primary Care. 2014;3(1):48-53. doi:10.4103/2249-4863.130275.
23. Madan N, Sharma S, Sood SK, Colah R, Bhatia LH. Frequency of β-thalassemia trait and other hemoglobinopathies in northern and western India. Indian J Hum Genet. 2010 Jan;16(1):16-25. doi: 10.4103/0971-6866.64941. [PubMed]
24. Kumar R, Singh K, Panigrahi I, Agarwal S. Genetic Heterogeneity of Beta Globin Mutations among Asian-Indians and Importance in Genetic Counselling and Diagnosis. Mediterr J Hematol Infect Dis. 2013;5(1):e2013003. doi: 10.4084/MJHID.2013.003. Epub 2013 Jan 2.
25. National Family Health Survey-3 (NFHS-3)-India 2005-06. Mumbai, International Institute for Population Sciences. 2005. [Last accessed on 2015 October 22]. http://rchiips.org/nfhs/NFHS-3%20Data/VOL-2/Report-%20Volume-II(1632K).pdf
26. Gomber S, Kumar S, Rusia U, Gupta P, Agarwal KN, Sharma S. Prevalence & etiology of nutritional anaemias in early childhood in an urban slum. Indian J Med Res. 1998 Jun;107:269-73. [PubMed]
27. Osório MM, Lira PI, Batista-Filho M, Ashworth A. Prevalence of anemia in children 6-59 months old in the state of Pernambuco, Brazil. Rev Panam Salud Publica. 2001 Aug;10(2):101-7. [PubMed]
28. Gomber S, Bhawna, Madan N, Lal A, Kela K. Prevalence & etiology of nutritional anaemia among school children of urban slums. Indian J Med Res. 2003 Oct;118:167-71. [PubMed]
29. Viswanath D, Hegde R, Murthy V, Nagashree S, Shah R. Red cell distribution width in the diagnosis of iron deficiency anemia. Indian J Pediatr. 2001 Dec;68(12):1117-9.
30. Kapoor D, Agarwal KN, Sharma S, Kela K, Kaur I. Iron status of children aged 9-36 months in an urban slum Integrated Child Development Services project in Delhi. Indian Pediatr. 2002 Feb;39(2):136-44. [PubMed]
31. Giebel HN, Suleymanova D, Evans GW. Anemia in young children of the Muynak District of Karakalpakistan, Uzbekistan: prevalence, type, and correlates. Am J Public Health. 1998 May;88(5):805-7. [PubMed]
32. Mitra SS. The clinical and hematological profile of thalassemia and hemoglobinopathies in India. Indian Pediatr. 1983 Oct;20(10):701-13.
Copyright (c) 2015 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


