Study on breast feeding and complementary feeding practices in rural mothers, Tamilnadu, India
Abstract
Introduction: Breast feeding of infants and young child is the natural and effective method which plays a major role in reducing the mortality of infants and under five children. There is significant reduction in the morbidities in the above age due to breast feeding. Inadequate knowledge and poor practices of breast feeding hinders the successful establishment of breast feeding.
Objective: To determine the breast feeding and complementary feeding practices of mothers with children of age below 3 years from rural area who visited the outpatient department of paediatrics of karpagavinayaga institute of medical sciences, Kancheepuram, Tamilnadu.
Materials and Methods: This was across sectional study done in hospital from 2017 September to 2018 January for a total duration of five months with structured questionnaire.
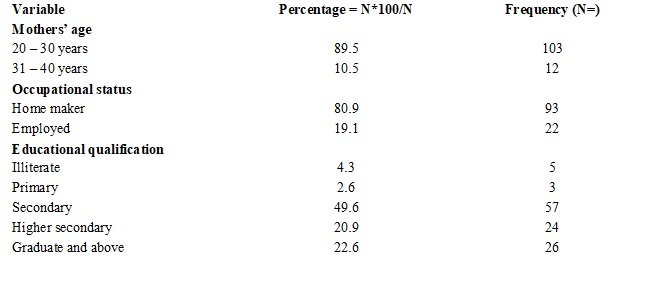
Results: Exclusive breast feeding was given to 68.7% (n=76) of children. About 69.5% of the mothers had initiated the breast feeding within one hour of delivery. About 89.6% had given colostrum. Prelacteal feeds were given in 10.4%. Only 32.2% of mothers fed their babies on demand. Complementary feeding was started after six months by 80.9% mothers. Complementary feeding was started with homemade food by 49.6% of mothers.
Conclusion: This study emphasis on education of mothers during their antenatal care, postnatal care and follow up care by obstetricians, paediatricians, residents and staff nurses regarding the importance of breast feeding and their advantages for better outcome in terms of reducing the morbidities and mortality in children below five years.
Downloads
References
2. James DC, Lessen R; American Dietetic Association. Position of the American Dietetic Association: promoting and supporting breastfeeding. J Am Diet Assoc. 2009 Nov;109(11):1926-42.[pubmed]
3. WHO and UNICEF. Global strategy for infant and young child feeding. World Health Organization, Geneva, 2003.Available at www.who.int/nutrition/publications/9241562218/en/.
4. Harnagle R, Chawla P S. A study of knowledge, attitude and practices of lactating mothers on breast feeding, weaning immunization and dietary practices at Jabalpur cantonment, India. Int. J. Microbiol. App. Sci. 2013;2(11): 393-403.
5. National Family Health Survey (NFHS-4). Factsheets 2015 - 2016. India: International Institute for Population Sciences. Available from URL: http://www.nfhsindia.org. Accessed on 9June 2017.
6. Som B, Tripura K. A cross-sectional study regarding knowledge about breastfeeding among primi pregnant mothers attending for antenatal check up in a medical college. Tripura. J. Evolution Med. Dent. Sci.2016;5(81):6061-3.
7. Edmond KM, Zandoh C, Quigley MA, et al. Delayed breastfeeding initiation increases risk of neonatal mortality. Pediatrics. 2006 Mar;117(3):e380-6. DOI:10.1542/peds.2005-1496.[pubmed]
8. Ministry of statistics and programme implementation. NewDelhi: Central statistics organization. Millennium Development Goals. Final country report of India Government of India. Available at URL:http://www.mospi.gov.in. Accessed on 19 February2019.
9. Shaili V, Parul S et al. A community based study on breastfeeding practices in a rural area of Uttarakhand. Nat JComm Med. 2012;3(2):283-7.
10. Dandekar RH, Shafee M, Kumar R. Breast feeding and weaning practices among literate mothers. The Health Agenda. 2014 ;2(1):15-25.
11. Ekubay M, Berhe A, Yisma E. Initiation of breastfeeding within one hour of birth among mothers with infants younger than or equal to 6 months of age attending public health institutions in Addis Ababa, Ethiopia. Int Breastfeed J. 2018 Jan 23;13:4. doi: 10.1186/s13006-018-0146-0. eCollection 2018.[pubmed]
12. Khan J, Vesel L, Bahl R, et al. Timing of breastfeeding initiation and exclusivity of breastfeeding during the first month of life: effects on neonatal mortality and morbidity--a systematic review and meta-analysis. Matern Child Health J. 2015 Mar;19(3):468-79. doi: 10.1007/s10995-014-1526-8.[pubmed]
13. Sharif M, Saxena A, Nair S, Sharma A, Jain P. Knowledge, attitude and practices of nursing mothers toward breastfeeding in a tertiary care center in Navi Mumbai. Indian J Child Health. 2017; 4(2):243-7.
14. Akuse RM, Obinya EA. Why healthcare workers give prelacteal feeds. Eur J Clin Nutr. 2002 Aug;56(8):729-34. DOI:10.1038/sj.ejcn.1601385.[pubmed]
15. Mandal PK, Sardar JC, Chatterjee C, Lahiri SK, Ghosh PK.Astudy on breast feeding practices among infants in a rural area of West Bengal. Indian J Prevand Soc Med. 2007; 38(1&2):28-31.
16. Lacovou M, Sevilla A. Infant feeding: the effects of scheduled vs. on-demand feeding on mothers' wellbeing and children's cognitive development. Eur J Public Health. 2013 Feb;23(1):13-9. doi: 10.1093/eurpub/cks012. Epub 2012 Mar 14.[pubmed]
17. Maiti A, Sarangi L. Assessment on breastfeeding and weaning practices in Odisha, India. Am J Pub Health Res. 2015;3(4A):49-52.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


