Comparison of Biomarkers of Neonatal Sepsis: Pro- Calcitonin Vs C-Reactive Protein
Abstract
Background: Procalcitonin in neonatal sepsis (NS) has high sensitivity compared to C-reactive protein (CRP), but its specificity is not yet clearly defined.
Objectives: Evaluation of Procalcitonin as an early marker, assessing its diagnostic utility in early-onset NS was the primary and comparing the levels of Procalcitonin with CRP was secondary objective.
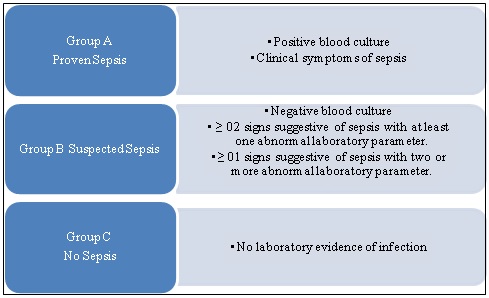
Method: In this observational, prospective study, neonates meeting the selection criteria were included and grouped into three, according to clinical symptoms of sepsis and blood culture.
Results: Blood samples from 75 babies (male = 61.0%) were analysed; 63.0% and 37.0% were of gestational age (GA) ≥ 37 and < 37 and weeks, respectively. Birth-weight< 2.5 kg and >2.5 Kg was noted in 52.0% and 48.0%, respectively. Meconium stained liquor (n=34), premature rupture of membranes (n=19) and prolonged labour/instrumental delivery (n=13) were major maternal risk factors.General (45.33%), respiratory (25.33%), gastrointestinal (17.33%), cardiovascular (6.66%)symptoms were common presentation; forty one (55.0%) were negative for procalcitonin and 34 (45.0%) were positive; 61 (81.0%) tested negative for CRP, only 14 (19.0%) were positive with levels >10mg/mL. Procalcitonin positivity was statistically significant (<0.05) for males, term babies and with normal birth weight favouring procalcitonin. of seven positive blood culture, coagulase positive staphylococci (n= 03), Klebsiella(n= 02), E. coli (n=01), Pseudomonas (n=01) were isolated. On correlation with blood culture, Procalcitonin showed better sensitivity and negative predictive value.
Conclusion: Procalcitoninis a better early marker than CRP in early onset NS. It hasbetter positivity for male, term and normal birth weight babies.
Downloads
References
2. National Neonatal Perinatal Database. Report 2002-03. Published by NNPD Nodal Centre, Department of Pediatrics, All India Institute of Medical Science, New Delhi. Available from http://www.newbornwhocc.org/ pdf/nnpd_report_2002-03.PDF last accessed 22 February 2019.
3. Vergnano S, Sharland M, Kazembe P, et al. Neonatal sepsis: an international perspective. Arch Dis Child Fetal Neonatal Ed. 2005 May;90(3):F220-4. DOI:10.1136/adc.2002.022863.[pubmed]
4. Da Silva O, Ohlsson A, Kenyon C. Accuracy of leukocyte indices and C-reactive protein for diagnosis of neonatal sepsis: a critical review. Pediatr Infect Dis J. 1995 May;14(5):362-6.[pubmed]
5. Camacho-Gonzalez A, Spearman PW, Stoll BJ. Neonatal infectious diseases: evaluation of neonatal sepsis. Pediatr Clin North Am. 2013 Apr;60(2):367-89. doi: 10.1016/j.pcl.2012.12.003. Epub 2013 Jan 17.[pubmed]
6. Squire E, Favara B, Todd J. Diagnosis of neonatal bacterial infection: hematologic and pathologic findings in fatal and nonfatal cases. Pediatrics. 1979 Jul;64(1):60-4.[pubmed]
7. Chauhan SB, Vaghasia V, Chauhan BB. C-reactive protein (crp) in early diagnosis of neonatal septicemia. National Journal of Medical Research 2012; 2(3):276–78.
8. Lakhey, A., & Shakya, H. Role of Sepsis Screening in early diagnosis of Neonatal Sepsis. Journal of Pathology of Nepal, 2017;7(1):1103-10. https://doi.org/10.3126/jpn.v7i1.16944.
9. Pontrelli G, De Crescenzo F, Buzzetti R, Jenkner A, Balduzzi S, et al. Accuracy of serum procalcitonin for the diagnosis of sepsis in neonates and children with systemic inflammatory syndrome: A meta-analysis. BMC Infect Dis.2017;17(1):302. doi: 10.1186/s12879-017-2396-7.
10. Indino P1, Lemarchand P, Bady P, de Torrenté A, Genné L, Genné D. Prospective study on procalcitonin and other systemic markers in patients with Leucocytosis. International J Infect Dis 2008; 12(3):319-24.
11. Angus DC, Wax RS. Epidemiology of sepsis: an update. Crit Care Med. 2001 Jul;29(7 Suppl):S109-16.[pubmed]
12. Benitz WE, Han MY, Madan A, et al. Serial serum C-reactive protein levels in the diagnosis of neonatal infection. Pediatrics. 1998 Oct;102(4):E41.[pubmed]
13. Altunhan H, Annagür A, Örs R, Mehmetoğlu I. Procalcitonin measurement at 24 hours of age may be helpful in the prompt diagnosis of early-onset neonatal sepsis. Int J Infect Dis. 2011 Dec;15(12):e854-8. doi: 10.1016/j.ijid.2011.09.007. Epub 2011 Oct 22.[pubmed]
14. Meem M, Modak JK, Mortuza R, et al. Biomarkers for diagnosis of neonatal infections: A systematic analysis of their potential as a point-of-care diagnostics. J Glob Health. 2011 Dec;1(2):201-9.[pubmed]
15. Ali AM, Moaz MA, Ghoniem E, et al. Reliability of serum procalcitonin concentrations for the diagnosis of sepsis in neonates. Egypt J Immunol. 2008;15(1):75-84.[pubmed]
16. Sucilathangam G, Amuthavalli K, Velvizhi G, Ashihabegum MA, Jeyamurugan T, Palaniappan N. Early Diagnostic Markers for Neonatal Sepsis: Comparing Procalcitonin (PCT) and C-Reactive Protein (CRP). Journal of clinical and diagnostic research 2012;6:627-631.
17. Guibourdenche J, Bedu A, Petzold L, et al. Biochemical markers of neonatal sepsis: value of procalcitonin in the emergency setting. Ann Clin Biochem. 2002 Mar;39(Pt 2):130-5. DOI:10.1258/0004563021901874.[pubmed]
18. Ballot DE, Perovic O, Galpin J, et al. Serum procalcitonin as an early marker of neonatal sepsis. S Afr Med J. 2004 Oct;94(10):851-4.[pubmed]
19. Mehar, V, Agarwal S, Singh R, Agarwal A, Agrawal N, Majethia A. Relationship between gestational age and mode of delivery with neonatal septicemia. International Journal of Contemporary Pediatrics,2016;3(3): 891-95. DOI: http://dx.doi.org/10.18203/2349-3291.ijcp20162361
20. Tallur SS, Kasturi AV, Nadgir SD, et al. Clinico-bacteriological study of neonatal septicemia in Hubli. Indian J Pediatr. 2000 Mar;67(3):169-74.[pubmed]
21. Kinchi YR, Kumar A,Yadav S. Profile of Neonatal sepsis.J Coll Med Sci Nepal 2010;6(2):1-6. https://doi.org/10.3126/jcmsn.v6i2.3609
22. Chacko B, Sohi I. Early onset neonatal sepsis. Indian J Pediatr. 2005 Jan;72(1):23-6.[pubmed]
23. Gallegher PG. Sepsis Neonatorum. In: McMillan JA, De Angelis C, Jones MD. OskisPediatrics Merck Manual; 2005.
24. Malik A, Hasani SE, Khan HM, et al. Nosocomial infections in newborns. Indian Pediatr. 2001 Jan;38(1):68-71.[pubmed]
25. Pérez RO, Lona JC, Quiles M, et al. [Early neonatal sepsis, incidence and associated risk factors in a public hospital in western Mexico]. Rev ChilenaInfectol. 2015 Aug;32(4):387-92. doi: 10.4067/S0716-10182015000500003.[pubmed]
26. Salem SY, Sheiner E, Zmora E, et al. Risk factors for early neonatal sepsis. Arch Gynecol Obstet. 2006 Jul;274(4):198-202. Epub 2006 Feb 21. DOI:10.1007/s00404-006-0135-1.[pubmed]
27. Tapia-Rombo CA, Cortés-Sauza J, Saucedo-Zavala VJ, Cuevas-Urióstegui ML. Predisposing risk factors that participate in neonatal sepsis mortality rate. Gac Med Mex. 2006;142(4):283-9.[article in Spanish].[pubmed]
28. Haque KN, Khan MA, Kerry S, et al. Pattern of culture-proven neonatal sepsis in a district general hospital in the United Kingdom. Infect Control Hosp Epidemiol. 2004 Sep;25(9):759-64. DOI:10.1086/502473
29. Raghavan M, Mondal GP, Bhat BV, et al. Perinatal risk factors in neonatal infections. Indian J Pediatr. 1992 May-Jun;59(3):335-40.[pubmed]
30. Kuruvilla KA, Pillai S, Jesudason M, et al. Bacterial profile of sepsis in a neonatal unit in south India. Indian Pediatr. 1998 Sep;35(9):851-8.[pubmed]
31. Mathai E, Christopher U, Mathai M, et al. Is C-reactive protein level useful in differentiating infected from uninfected neonates among those at risk of infection? Indian Pediatr. 2004 Sep;41(9):895-900.[pubmed]
32. Boyle RJ, Chandler BD, Stonestreet BS, et al. Early identification of sepsis in infants with respiratory distress. Pediatrics. 1978 Nov;62(5):744-50.[pubmed]
33. Rodwell RL, Anton LL, David IT. Early diagnosis of Neonatal sepsis using a haematological scoring system. J Pediatr 1987; 112(5): 761-7.
34. Roy I, Jain A, Kumar M, et al. Bacteriology of neonatal septicaemia in a tertiary care hospital of northern India. Indian J Med Microbiol. 2002 Jul-Sep;20(3):156-9.[pubmed]
35. Ahmed AS, Chowdhury MA, Hoque M, et al. Clinical and bacteriological profile of neonatal septicemia in a tertiary level pediatric hospital in Bangladesh. Indian Pediatr. 2002 Nov;39(11):1034-9.[pubmed]
36. Karthikeyan G, Premkumar K. Neonatal sepsis: Staphylococcus aureus as the predominant pathogen. Indian J Pediatr. 2001 Aug;68(8):715-7.[pubmed]
37. Kumhar GD, Ramachandran VG, Gupta P. Bacteriological analysis of blood culture isolates from neonates in a tertiary care hospital in India. J Health PopulNutr. 2002 Dec;20(4):343-7.[pubmed]
38. Joram N, Boschar C, Denizot S, V Loubersac, N Winer, J C Rose et al. Umbilical cord blood procalcitonin and C reactive protein concentrations as markers for early diagnosis of very early-onset neonatal infection.Arch Dis Child Fetal Neonatal Ed. 2006; 91(1): 65-6.
39. Abdollahi A1, Shoar S, Nayyeri F, et al. Diagnostic Value of Simultaneous Measurement of Procalcitonin, Interleukin-6 and hs-CRP in Prediction of Early-Onset Neonatal Sepsis. Mediterr J Hematol Infect Dis. 2012;4(1):e2012028. doi: 10.4084/MJHID.2012.028. Epub 2012 May 6.
40. Bonac B, Derganc M, Wraber B, et al. Interleukin-8 and procalcitonin in early diagnosis of early severe bacterial infection in critically ill neonates. Pflugers Arch. 2000;440(5 Suppl):R72-4.[pubmed]
41. Naher BS, Mannan MA, Noor K, et al. Role of serum procalcitonin and C-reactive protein in the diagnosis of neonatal sepsis. Bangladesh Med Res Counc Bull. 2011 Aug;37(2):40-6.[pubmed]
42. Vazzalwar R, Pina-Rodrigues E, Puppala BL, et al. Procalcitonin as a screening test for late-onset sepsis in preterm very low birth weight infants. J Perinatol. 2005 Jun;25(6):397-402.[pubmed]
43. Janota J, Stranák Z, Bĕlohlávková S, et al. Postnatal increase of procalcitonin in premature newborns is enhanced by chorioamnionitis and neonatal sepsis. Eur J Clin Invest. 2001 Nov;31(11):978-83.[pubmed]
44. Köksal N, Harmanci R, Cetinkaya M, et al. Role of procalcitonin and CRP in diagnosis and follow-up of neonatal sepsis. Turk J Pediatr. 2007 Jan-Mar;49(1):21-9.[pubmed]
45. Fendler WM, Piotrowski AJ. Procalcitonin in the early diagnosis of nosocomial sepsis in preterm neonates. J Paediatr Child Health. 2008 Mar;44(3):114-8. Epub 2007 Oct 10. DOI:10.1111/j.1440-1754.2007.01230.x
46. Lachowska M, Gajewska E. Usefulness of procalcitonin (PCT) as a marker of early-onset systemic infections in preterm newborns. Med Sci Monit. 2004; 10(Suppl 2): 33-5.
47. Baltimore RS. Neonatal sepsis: epidemiology and management. Paediatr Drugs. 2003;5(11):723-40. DOI:10.2165/00148581-200305110-00002.[pubmed]
48. Chauhan N, Tiwari S, Jain U. Potential biomarkers for effective screening of neonatal sepsis infections: An overview. MicrobPathog. 2017;107:234-42. doi: 10.1016/j.micpath.2017.03.042.
49. Qiu X1, Zhang L1, Tong Y, et al. Interleukin-6 for early diagnosis of neonatal sepsis with premature rupture of the membranes: A meta-analysis. Medicine (Baltimore). 2018 Nov;97(47):e13146. doi: 10.1097/MD.0000000000013146.[pubmed]
50. Hahn WH, Song JH, Kim H, et al. Is procalcitonin to C-reactive protein ratio useful for the detection of late onset neonatal sepsis? J MaternFetal Neonatal Med. 2018 Mar;31(6):822-826. doi: 10.1080/14767058.2017.1297410. Epub 2017 Mar 9.[pubmed]
51. Stocker M, van Herk W, El Helou S, et al. Procalcitonin-guided decision making for duration of antibiotic therapy in neonates with suspected early-onset sepsis: a multicentre, randomised controlled trial (NeoPIns). Lancet. 2017 Aug 26;390(10097):871-881. doi: 10.1016/S0140-6736(17)31444-7. Epub 2017 Jul 12.[pubmed]
Copyright (c) 2019 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


