Clinico-laboratory profile of Seropositive Celiac Diseases in Severe Acute Malnutrition
Abstract
Introduction: Celiac Disease shares clinical features with malnutrition and may be responsible for malnutrition. The objective of this study was to study clinico-laboratory profile of seropositive Celiac Diseases in Severe Acute Malnutrition.
Material & Methods: The present study was a prospective, hospital based, observational study conducted at Malnutrition Treatment Centre (MTC) of tertiary care Pediatric hospital associated with government medical college of southern Rajasthan. The study was conducted over the period of one year from Dec. 2017 to Nov. 2018. Total 110 children with Severe Acute Malnutrition enrolled and screened for Celiac Disease on the basis of celiac serology (tTg-IgA/IgG). Clinico-laboratory findings of celiac seropositive and seronegative patients were recorded and analysed statistically.
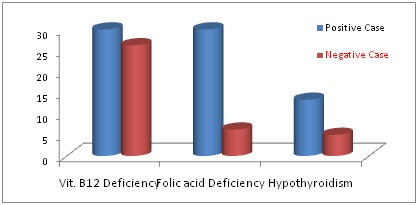
Results: Celiacsero-positivity was observed in 30 cases (27.28%). Out of these seropositive cases 14 cases (46.66%) were seropositive for both tTg-IgA and IgG, while 9 cases (30%) were positive for only tTg-IgA and rest 7 cases (23.33%) were positive for only tTg-IgG. Most of the seropositive patients (12, 40%) were in age group of 4-5 years of age group. In seropositive cases recurrent blood in stool (54.45%) and recurrent diarrhoea (52.94%) were common clinical features at the time of admission. S. Vit. B12 & Folic Acid were low in all the patients but more seropositive patients showed low levels of S. Folic acid (P value <0.05).
Conclusions: Recurrent diarrhoea and blood in stool were common presenting feature on admission in celiac seropositive patients suffering from severe acute malnutrition. Vit. B12 and Folic acid deficiency were also observed as a common finding in seropositive patients.
Downloads
References
2. Bhatnagar S, Tandon N. et al. Diagnosis of celiac disease. Indian J Pediatr. 2006 Aug;73(8):703-9.[pubmed]
3. Hu WT, Murray JA, Greenaway MC, et al. Cognitive impairment and celiac disease. Arch Neurol. 2006 Oct; 63(10):1440-6.[pubmed]
4. Cooke WT, Smith WT. Neurological disorders associated with adult Celiac Disease. Brain.1966;89 (4):683-22. https://doi.org/10.1093/brain/89.4.683.
5. Marks J, Shuster S, Watson A. Small-bowel changes in dermatitis herpetiformis. The Lancet. 1966;2 (7476):1280-82.DOI: https://doi.org/10.1016/S0140-6736(66)91692-8
6. Pengiran Tengah DS, Wills AJ, Holmes GK. Neurological complications of coeliac disease. Postgrad Med J. 2002 Jul; 78(921):393-8.[pubmed]
7. Hadjivassiliou M, Grunewald RA, Davies-Jones GA. Gluten Sensitivity as a neurological illness. J Neurol Neurosurg Psychiatry.2002;72 (5):560-63.doi: 10.1136/jnnp.72.5.560.
8. NetoJIS, Costa AC, Magalhaes FG, Silva GS. Neurological manifestations of Celiac Disease. Arch Neuropsiquiatr.2004;62:969-72. http://dx.doi.org/10.1590/S0004-282X2004000600007
9. Reilly NR, Green PH. Epidemiology and clinical presentations of celiac disease. Semin Immunopathol. 2012 Jul;34(4):473-8. doi: 10.1007/s00281-012-0311-2. Epub 2012 Apr 24.[pubmed]
10. Khoshoo V, Bhan MK, Jain R, et al. Coeliac disease as cause of protracted diarrhoea in Indian children. Lancet. 1988 Jan 16;1(8577):126-7.[pubmed]
11. Patwari AK, Anand VK, Kapur G, et al. Clinical and nutritional profile of children with celiac disease. Indian Pediatr. 2003 Apr;40(4):337-42.[pubmed]
12. García-Manzanares A, Lucendo AJ. Nutritional and dietary aspects of celiac disease. Nutr Clin Pract. 2011 Apr;26(2):163-73. doi: 10.1177/0884533611399773.[pubmed]
13. Caruso R, Pallone F, Stasi E, Romeo S, Monteleone G. Appropriate nutrient supplementation in Celiac Disease. Annals of Medicine.2013;45(8): 522-31. doi: 10.3109/07853890.2013.849383. Epub 2013 Nov 7.[pubmed]
14. Kumar P, Mishra K, Singh P, Rai K. Should we screen children with severe acute malnutrition for celiac disease? Indian Pediatr. 2012;49(4):330-31.
15. Beniwal N, Ameta G, Chahar CK. Celiac Disease in children with severe acute malnutrition (SAM) a hospital-based study. Indian J Pediatr. 2017;84(5):339-43.[pubmed]
16. Singh S, Shekhar C, Acharya R, et al. The incidence of abortion and unintended pregnancy in India, 2015. Lancet Glob Health. 2018 Jan;6(1):e111-e120. doi: 10.1016/S2214-109X(17)30453-9.[pubmed]
17. Aesku. Diagnostics. Aeskulisa- Instruction Manual: tTG new generation (Ref 3503/3504) available atwww.aesku.com [Last accessed on Nov. 20, 2018]
18. Sharma M, Mandot S. Prevalence and clinical profile of celiac disease among malnourished children in South Rajasthan, India. Int J Contemp Pediatr. 2018;5(3):997-1002. DOI: http://dx.doi.org/10.18203/2349-3291.ijcp20181529
19. Centers for Disease Control and Prevention. Available at: www.cdc.gov/nchc/data/nhans-0304/106-c-metfolates%20B12.pdf.[pubmed]
20. Lerner NB. Folic Acid Deficiency. In: Kliegman RSM, Stanton BF, St. Geme III JW, editors. Nelson Textbook of Pediatrics 20th edition, Philadelphia Elsevier, 2016: p-2319-23.
21. La Franchi SH, Huang SA. Hypothyroidism. In: Kliegman RM, Stanton BF, St. Geme III JW, editors. Nelson Textbook of Pediatrics 20th edition. Philadelphia Elsevier, 2016: p 2665-74.
Copyright (c) 2019 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


