A Prospective Study on the Clinical Features of Hyponatremic Dehydration in Acute Gastroenteritis
Abstract
Introduction:Babies and children with gentle lack of hydration regularly have negligible or no clinical changes other than a lessening in pee yield. Alongside diminished pee yield in kids with moderate drying out regularly have dried mucous layers, diminished skin turgor, crabbiness, tachycardia with diminished hair like refill, and profound breath.
Methodology: The study was done in Deccan College of Medical Sciences & Owaisi Group of Hospitals. Study population consisted from Infants to children aged till 12 years attending the paediatric Department both OPD and IPD care for acute gastroenteritis are enroll in the study. Aims and
Objectives: To estimate the incidence of hyponatraemic dehydrationin neonates and children. To evaluates the clinical features associated with acute gastroenteritis associated dehydration.
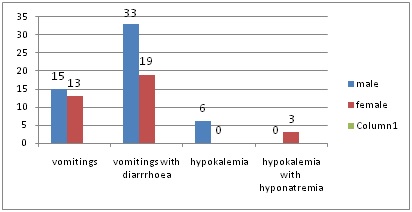
Results:80 cases were studied and analyzed to detect Gastroenteritis associated dehydration and its clinical features as a possible risk factor for hyponatremia. It was found that 60% of the males were having acute gastroenteritis while it was 40% in female subjects. The data also reveals that higher incidence of acute GE was noted between 6 to 24 months of age while the lower incidence was found in the subjects above 36 months of age.
Conclusion: The clinical impression of the type of dehydration and electrolyte disturbances was fairly consistent with serum electrolytes values. This suggest that routine estimation of serum electrolytes is not necessary however it is necessary whenever electrolyte imbalance is suspected on clinical grounds and in cases which do not respond satisfactorily with routine fluid electrolyte therapy.
Downloads
References
2. Dr. Peter Allan &Dr.SaibalGanguly, ATOTW 314 – Hyponatraemia (2nd April 2015) , Tutorial 314, Page1-8.
3. Karen S. Powers, Dehydration: Isonatremic, Hyponatremic, and Hypernatremic Recognition and Management. Pediatrics in Review, 2015 July 36 (7): 274-422.[pubmed]
4. Jacob J, Joseph TK, Srinivasan R, et al. Direct and Indirect Costs of Pediatric Gastroenteritis in Vellore, India. Indian Pediatr. 2016 Jul 8;53(7):642-4.[pubmed]
5. Spiros Fourlanos, Peter Greenberg. Managing drug-induced hyponatraemia in adults. Australian Prescriber, 2003 Vol. 26 ( 5): 114-117.
6. Das, Jagadish. (2015). Hypernatremic Dehydration in Newborn Infants: A Review. Ulutas Med J2015;1(2):22-25. DOI: 10.5455/umj.201506181158472.
7. Soiza, R. L., Cumming, K., Clarke, J. M., Wood, K. M., &Myint, P. K. (2014). Hyponatremia: Special Considerations in Older Patients. Journal of clinical medicine, 3(3), 944–958. doi:10.3390/jcm3030944.
8. Braun MM, Barstow CH, Pyzocha NJ. Diagnosis and management of sodium disorders: hyponatremia and hypernatremia. Am Fam Physician. 2015 Mar 1;91(5):299-307.[pubmed]
9. Arieff AI, Guisado R. Effects on the central nervous system of hypernatremic and hyponatremic states. Kidney Int. 1976 Jul;10(1):104-16.[pubmed]
10. Sahay M, Sahay R. Hyponatremia: A practical approach. Indian J Endocrinol Metab. 2014 Nov;18(6):760-71. doi: 10.4103/2230-8210.141320.[pubmed]
Copyright (c) 2019 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


