Effectiveness of predicting outcome in septic shock in critically ill children by assessing serum lactate levels
Abstract
Background and Aims: Hyperlactatemia at the time of admission is a documented risk factor for mortality in critically ill adult patients. However, the significance of lactate measurement at admission for mortality in critically ill children remains uncertain. This study evaluated the predictive value of blood lactate levels at the time of admission and determined the cut-off values for predicting in-hospital mortality in the critically ill children.
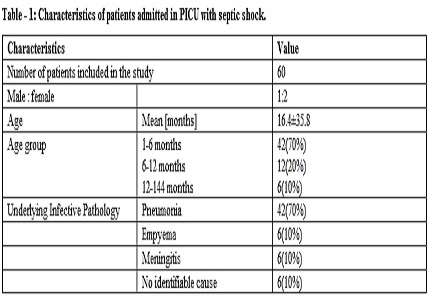
Materials and Methods: A total of 60 children with diagnosis of sepsis admitted to PICU of a tertiary care hospital were included in the study. PRISM III score and demographic characteristics of all children were recorded. Serum lactate levels were measured at 0-3, 12 and 24 h of PICU admission. The outcome like survival or death was correlated with serum lactate levels.
Results: Septic shock was the most common type of shock and had highest mortality. Lactate levels were significantly higher in non survivors in comparison to survivors. A lactate value of more than 5 mmol/l at 0-3, 12 and 24h of PICU admission had increased mortality.
Conclusions: A high blood lactate level at admission is independently associated with higher in-hospital mortality in the critically ill children.
Downloads
References
2. Carcillo JA, Fields AI. Task force Committee Members, Clinical Practice parameters for hemodynamic support of pediatric and neonatal patients in septic shock. Crit care Med 2002;30:1365-78.
3. Mizock BA. The hepatosplanchnic area and hyperlacatatemia: A tale of two lactates. Crit care Med 2001;29:442-59. [PubMed]
4. Stacpolle PW. Lactic acidosis. Endocrinol Metabol Clin North Am 1993;22:221-45. [PubMed]
5. Valenza F, Aletti G, Fossali T, Chevallard G, Sacconi F, Irace M, et al. Lactate as a marker of energy failure in critically ill patients: Hypothesis. Critical Care 2005;9:588-93. [PubMed]
6. Deshpande SA, Ward-Platt MP. Association between blood lactate and acid-base status and mortality in ventilated babies. Arch Dis Child Fetal Neonatal Ed 1997;76:F15-20. [PubMed]
7. Fitzgerald MJ, Gota M, Myers TF, Zeller WP. Early metabolic effects of sepsis in the preterm infant: Lactic acidosis and increased glucose requirement. J Pediatr 1992;121:951-5. [PubMed]
8. RPhillipDellinger,MitchelMLevy,AndrewRoads,SurvivingSepsis Campaign.International Guideline for Management of Severe sepsis and Setic shock 2012.
9. R N Taori,Keya R,S Tullu Performance of PRISM(pediatric risk of mortality) score and PIM (pediatric risk of mortality) score in tertiary care pediatric ICU. Indian journal of pediatrics,vol-77,mar2010 [PubMed]
10. Pollack MM, Patel KM, Ruttimann UE. PRISM III: An updated pediatric risk of mortality score. Crit Care Med 1996;24:743-52. [PubMed]
11. Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R et al. Survivings Sepsis Campaign: International guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med 2008;36:296-327.
12. Duke TD, Butt W, South M. Predictors of mortality and multiple organ failure in children with sepsis. Intensive Care Med 1997;23:684-92. [PubMed]
13. Hatherill M, Mclntyre AG, Wattie M, Murdoch AI. Early hyperlactatemia in critically ill children. Intensive Care Med 2000;26:314-8. [PubMed]
14. Jacobs RF, Sowell MK, Moss MM. Septic shock in children: Bacterial etiologies and temporal relationship. Pediatr Infect Dis J 1990;9:196-200. [PubMed]
15. Carcillo JA, David AL, Zaritsky A. Role of early fluid resuscitation in pediatric septic shock. JAMA 1991;266:1242-5. [PubMed]
16. Mikkelsen ME, Miltiades AN, Gaieski DF, Goyal M, Funhs BD, Shah CV, et al. Serum lactate is associated with mortality in sever sepsis independent of organ failure and shoc. Crit Care Med 2009;37:1670-7. [PubMed]
17. Bernardin G, Pradier C, Tiger F, Deloffre P, Mattei M. Blood pressure and arterial lactate level are early indicators of short term survival in human septic shock. Intensive Care Med 1996;22:17-25. [PubMed]
18. Marecaux G, Pinsky MR, Dupont E, Kahn RJ, Vincent JL. Blood lactate levels are better prognostic indicators than TNF and IL-6 levels in patient with septic shock. Intensive Care Med 1996;22:404-8. [PubMed]
19. Nguyen HB, Rivers EP, Knoblich BP, Jacobsen G, Muzzin A, Ressler JA, et al. Early lactate clearance is associated with improved outcome is severe sepsis and septic shock. Crit Care Med 2004;32:1637-42.
Copyright (c) 2016 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


