Hemophilia in children: a clinico-epidemiological profile and review
Abstract
Introduction: Objective: To describe the clinical and epidemiological profile of hemophilia patients in the pediatric age group at a tertiary care center in Western Uttar Pradesh.
Materials and Methods: This was an observational cross-sectional study that was conducted at the Department of Pediatrics, S.N. Medical College, Agra. Pediatric patients (0-18 years) with hemophilia admitted in the Pediatrics emergency ward for Anti- Hemophilic factor transfusion or having a history of such type of transfusion during the year 2018-19 were consecutively enrolled in the present study. A detailed clinical history was taken from the parent or guardian accompanying the case.
Results: Out of the total 93 pediatric hemophilia patients, the majority 61% (57/93) belonged to 11 to 18 years of age group. 2.1% (2/93) were< 1 year of age. 17.2 % (16/93) were in 1-5 years of age group. 19.35% were in 6-10 years of age group. Out of the total, 98.9% (92/93) were males while only 1.07% (1/93) were female. Type A hemophilia was observed in 87.09% (81/93) patients while Type B hemophilia was present in only 12.9% (12/93) patients. Out of 81 Type-A hemophilia patients, only one had developed Inhibitor (1.07%). None among Type B hemophilia patients had Inhibitors. Out of total cases, only one patient (1.07%) had von Willebrand Deficiency.91%(85/93) patients presented with joint bleed. The knee joint was the most commonly affected joint, as observed in 64.7% (55/85) patients.
Conclusion: A better insight into the disease prevalence is pivotal for early diagnosis and to provide quality care to all hemophilia patients. The development of an inhibitor is a major concern. Physiotherapy and RICE(Rest, Ice, Compression and elevation) should be emphasized for the better quality of life and preventing joint hemarthrosis.
Downloads
References
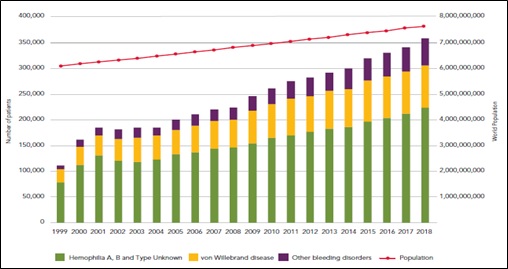
World Federation of Hemophilia. Report on the Annual Global Survey 2018.Montreal, Canada: WFH,2019. Available at http://www1.wfh.org/publications/files/pdf-1714.pdf.
Davies J, Kadir RA. Mode of delivery and cranial bleeding in newborns with haemophilia: A systematic review and meta-analysis of the literature. Haemophilia. 2016;22(1):32-38. doi: https://doi.org/10.1111/hae.12726.
Payal V, Sharma P, Goyal V, Jora R, Parakh M, Payal D. Clinical profile of hemophilia patients in Jodhpur region. Asian J Transfus Sci. 2016;10(1):101-104. Available from: http://www.ajts.org/text.asp?2016/10/1/101/164269
Witmer C, Young G. Factor VIII inhibitors in hemophilia A: rationale and latest evidence. Ther Adv Hematol. 2013;4(1):59-72. doi: https://doi.org/10.1177/2040620712464509.
Paroskie A, Gailani D, DeBaun MR, Sidonio RF Jr. A cross-sectional study of bleeding phenotype in haemophilia A carriers. Br J Haematol. 2015;170(2):223-228. doi: https://doi.org/10.1111/bjh.13423.
Kamal AH, Tefferi A, Pruthi RK. How to interpret and pursue an abnormal prothrombin time, activated partial thromboplastin time, and bleeding time in adults. Mayo Clin Proc. 2007;82(7):864-873. doi: https://doi.org/10.4065/82.7.864.
World Federation of Hemophilia. Report on the Annual Global Survey 2017.Montreal, Canada: WFH,2018. Available at http://www1.wfh.org/publications/files/pdf-1714.pdf.
World Federation of Hemophilia. Annual Global Survey, Mini Report 1. WHF, April 2017. Available at http://www1.wfh.org/publications/files/pdf-1680.pdf.
James AH, Kouides PA, Abdul-Kadir R, Edlund M, Federici AB, Halimeh S, et al. Von Willebrand disease and other bleeding disorders in women: consensus on diagnosis and management from an international expert panel. Am J Obstet Gynecol. 2009;201(1):12-e1.
World Federation of Hemophilia. Report on the Annual Global Survey 2015. Montreal, Canada: WFH, 2016. Available at https://www1.wfh.org/publications/files/pdf-1690.pdf.
Srivastava A, Brewer AK, Mauser-Bunschoten EP, Key NS, Kitchen S, Llinas A, et al. Guidelines for the Management of Hemophilia. Haemophilia. 2013;19(1):1-4. doi: https://doi.org/10.1111/j.1365-2516.2012.02909.x.
Ananyeva NM, Lee TK, Jain N, Shima M, Saenko EL. Inhibitors in hemophilia A: advances in elucidation of inhibitory mechanisms and in inhibitor management with bypassing agents. Semin Thromb Haemost. 2009; 35(8):735-751. doi: https://doi.org/10.1055/s-0029-1245106.
Santagostino E, Morfini M, Auerswald GK-H, et al. Paediatric haemophilia with inhibitors: existing management options, treatment gaps and unmet needs. Haemophilia.2009;15(5):983-989.
Wight J, Paisley S. The epidemiology of inhibitors in haemophilia A: a systematic review. Haemophilia.2003;9(4):418-435. doi: https://doi.org/10.1046/j.1365-2516.2003.00780.x.
Gouw SC, van den Berg HM. The multifactorial etiology of inhibitor development in hemophilia: genetics and environment. Semin Thromb Haemost. 2009;35(8):723-734. doi: https://doi.org/10.1055/s-0029-1245105.
Mishra S, Kumar S, Panwar A, Bhagchandani D, Aneja GK, Verma N, et al. A clinical profile of hemophilia patients and assessment of their quality of life in Western Uttar Pradesh, India: an observational study. Med J DY Patil Univ. 2016;9(3):320-324. doi: https://doi.org/10.4103/0975-2870.182501
Agarwal MB, Mehta BC, Bhanotra PC. Classical hemophilia a study of 236 cases from 212 unrelated families. J Assoc Physicians India. 1981;29(5):385-389.
Kulkarni R, Soucie JM, Lusher J, Presley R, Shapiro A, Gill J, et al. Sites of initial bleeding episodes, mode of delivery and age of diagnosis in babies with haemophilia diagnosed before the age of 2 years: a report from the centers for disease control and prevention’s (CDC) universal data collection (UDC) project. Haemophilia. 2009;15(6):1281-1290. doi: https://doi.org/10.1111/j.1365-2516.2009.02074.x.
Kar A, Mirkazemi R, Singh P, Potnis-Lele M, Lohade S, Lalwani A, et al. Disability in Indian patients with haemophilia. Haemophilia. 2007;13(4):398-404. doi: https://doi.org/10.1111/j.1365-2516.2007.01483.x.
Wight J, Paisley S. The epidemiology of inhibitors in haemophilia A: a systematic review. Haemophilia. 2003;9(4):418-435. doi: https://doi.org/10.1046/j.1365-2516.2003.00780.x.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


