Morbidity and Mortality pattern in Neonatal ICU in a tertiary care teaching hospital of Puducherry, South India
Abstract
Objectives: This study was undertaken to know about the morbidity and mortality pattern of neonates admitted in neonatal ICU in a tertiary care teaching hospital.
Materials and Methods: This is a hospital-based, retrospective, descriptive study, done on newborns admitted to neonatal ICU of Sri Venkateshwara Medical College Hospital and Research Centre, Puducherry from January 2018-December 2019 (24 months).
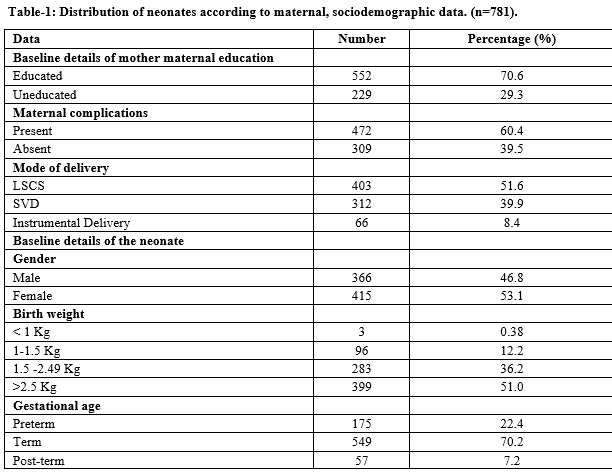
Results: As about 935 neonates were admitted to neonatal ICU. About 781 neonates were analyzed. Maternal details showed that (70.6%) were educated and (29.3%) of them were uneducated. Morbidity pattern studied in 773 (98.9%) neonates showed that, neonatal jaundice (19.2%), neonatal sepsis (12.1%), TTNB (11.7%), HIE (10.9%), RDS (10.3%), was the common reason for admission. Feeding difficulties were observed in (6.5%), IDM for blood glucose monitoring (5.9%), LBW/preterm care (5.1%), meningitis (2.9%), seizures (2.7%), NEC (2.4%), MAS (2.1%), congenital anomalies (1.9%). The outcome noted in the morbidity pattern was that 99.7% were discharged and 0.25% were referred. Analysis of mortality pattern 8(1.02%) showed that, according to birth weight <1 kg (37.5%) was the most common cause of death, followed by 1-1.5 kg (25%), 1.5 -2.49 kg (25%), > 2.5 kg (12.5%). Maternal complications contributing to neonatal mortality was observed in (75%), it was not seen in (25%). The cause of death noted was prematurity with RDS and sepsis in (62.5%), septic shock with MODS in (12.5%), aspiration pneumonitis (12.5%), prematurity with HIE and pulmonary hemorrhage (12.5%).
Conclusion: Neonatal jaundice, neonatal sepsis being the most common etiology for neonatal morbidity. Measures should be taken to diagnose jaundice earlier in high-risk cases. Steps should be taken to control neonatal sepsis by following sterile precautions during delivery. Prematurity and ELBW are the leading cause of neonatal mortality.
Downloads
References
Paul VK, Bagga A. GHAI essential pediatrics. CBS Publishers and Distributors. 2018. Available at https://medicostimes.com/op-ghai-essential-of-pediatrics-textbook-pdf/
UNICEF. The state of Worlds children. UNICEF, 2008:4-114. Available at https://www.unicef.org/publications/index_42623.html.
Lawan JE, Cousens S, Zupen J. 4 million neonatal deaths: When? Where? Why?. Lancet. 2005;365(9462):891-900. doi: https://doi.org/10.1016/s0140-6736(05)71048-5.
Modi R, Modi B, Patel JK, Punitha KM. Study of the Morbidity and the Mortality Pattern in the Neonatal Intensive Care Unit at a Tertiary Care Teaching Hospital in Gandhinagar District, Gujarat, India. J Res Med Den Sci. 2015;3(3):208-212. doi: https://doi.org/10.5455/jrmds.20153311.
Kapoor RK, Srivastava AK, Misra PK, Sharma B, Thakur S, Srivastava KL, et al. Perinatal Mortality in Urban Slums in Lucknow. Indian Pediatr. 1996;33(1):19-23.
Rasul CH, Hussain MA, Siddiquey AHM, Rahman MS. Perinatal mortality in a teaching hospital. Indian Pediatr. 1999;36(4):389-390.
Ranjan A, Singh A. Pattern of morbidity and mortality of neonates admitted in tertiary level neonatal intensive care unit in Nalanda Medical College and Hospital, Patna, Bihar, India. Int J Contemp Pediatr. 2016;3(3):854-857. doi: http://dx.doi.org/10.18203/2349-3291.ijcp20162355.
Kannan R, Rao S, Mithra P, Rajesh SM, Unnikrishnan B, Rekha T. Neonatal mortality and morbidity in a tertiary care hospital of coastal south India. J Nepal Paediatr Soc. 2017;37(3):232-237. doi: http://dx.doi.org/10.3126/jnps.v37i3.18734.
Tran HT, Doyle LW, Lee KJ, Graham SM. A systematic review of the burden of neonatal mortality and morbidity in the ASEAN Region. WHO South East Asia J Public Health. 2012;1(3):239-248. doi: http://doi.10.4103/22243151.207020.
Sangamam R. Perinatal mortality and morbidity among low birth weight babies. Int J Community Med Public Health. 2015;2(1):51-58. doi: http://doi:10.5455/2394-6040.ijcmph20150211.
Bhutta ZA, Das JK, Bahl R, Lawn JE, Salam RA, Paul VK, et al. Can available interventions end preventable deaths in mothers, newborn babies, and stillbirths, and at what cost?. Lancet. 2014;384(9940):347-370. doi: https://doi.org/10.1016/S0140-6736(14)60792-3.
Tomo BO, Ige OO, Abok II, Onwuanaku C, Abah RO, Donli A. Pattern of neonatal admissions and outcome in a tertiary institution in north central Nigeria.J Med Trop. 2019;15(2):121-125. Available from http://www.jmedtropics.org/text.asp?2013/15/2/121/123590.
Shrestha M, Manandhar DS, Dhakal S, Nepal N. Two-year audit of perinatal mortality at Kathmandu Medical College Teaching Hospital. Kathmandu Univ Med J. 2006;4(2):176-181.
Manandhar SR, Manandhar DS, Baral MR, Pandey S, Pandhey S. One-year audit of perinatal mortality at Kathmandu Medical CollegeHospital. Kathmandu Univ Med J. 2004;2(3):198-202.
Elmi Farah A, Abbas AH, Tahir Ahmed A. Trends of admission and predictors of neonatal mortality: A hospital based retrospective cohort study in Somali region of Ethiopia. PLoS ONE. 2018;13(9):e0203314. https://doi.org/10.1371/journal.pone.0203314.
Lawn JE, Blencowe H, Oza S, You D, Lee AC, Waiswa P, et al. Every Newborn: progress, priorities, and potential beyond survival. Lancet. 2014;384(9938):189-205. doi: https://doi.org/10.1016/s0140-6736(14)60496-7.
Veloso FCS, Kassar LML, Oliveira MJC, Lima THB, Bueno NB, Gurgel RQ et al. Analysis of neonatal mortality risk factors in Brazil: a systematic review and meta-analysis of observational studies. J Pediatr (Rio J). 2019;95(5):519-530. doi: https://doi.org/10.1016/j.jped.2018.12.014.
Sridhar PV, Thammanna PS, Sandeep M. Morbidity Pattern and Hospital Outcome of Neonates Admitted in a Tertiary Care Teaching Hospital, Mandya. Int J Sci Stud. 2015;3(6):126-129. doi: https://doi.org/10.17354/ijss/2015/407.
Saharia NP, Deka A, Vivekananda MS. Mortality and Morbidity Pattern of Neonatal ICU of Gauhati Medical College and Hospital. IOSR J Dent Med Sci. 2016;15(6)73-75. doi: https://doi.org/10.9790/0853-1506117375.
Modi R, Modi B, Patel J. Comparison of Neonatal Morbidity and Mortality among Late Preterm and Term Neonates at Neonatal Intensive Care in Gujarat. Nat J Community Med. 2015;6(4):483-486. doi: https://doi.org/10.5455/jrmds.20153311.
Saini N, Chhabra S, Chhabra S, Garg L, Garg N. Pattern of neonatal morbidity and mortality: A prospective study in a district Hospital in Urban India. J Clin Neonatol 2016;5(3):183-188. doi: https://doi.org/10.4103/2249-4847.191258.
Aluvaala J, Okello D, Murithi G, Wafula L, Wanjala L, Isika N et al. Delivery outcomes and patterns of morbidity and mortality for neonatal admissions in five Kenyan hospitals. J Trop Pediatr.2015;61(4):255-259. doi: https://dx.doi.org/10.1093%2Ftropej%2Ffmv024.
Cupen K, Barran A, Singh V, Dialsingh I. Risk Factors Associated with Preterm Neonatal Mortality: A Case Study Using Data from Mt. Hope Women’s Hospital in Trinidad and Tobago. Children (Basel). 2017;4(12):108. doi: https://dx.doi.org/10.3390%2Fchildren4120108.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


