Organisms causing urinary tract infections in children and their sensitivity pattern in a level 2 pediatric hospital at a district place in South India
Abstract
Background: Urinary Tract Infection is second the common bacterial infection affecting children. Resistance to routine antibiotics for treating CA-UTI is on the rise. It is necessary to determine the antibiotic sensitivity patterns of uropathogensin a particular region to prevent complications of UTI and to determine empirical antibiotic.
Aims: To evaluate the bacteriological profile and antibiotic sensitivity patterns in children with urinary tract infections
Setting and Design: Retrospective observational study conducted over a period of 2 years in a level 2 pediatric hospital at a district place in South India
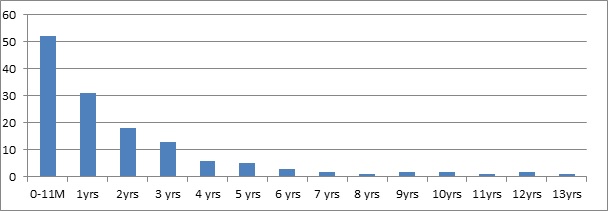
Materials and methods: Children between the ages of one day and 13 years who had UTI over a period of 2 years from 01 Jan 2018 to 31 Dec 2019 were included in the study. Urine specimens with the growth of single organism of >105/ml were studied forvariousuropathogens and their sensitivity patterns.
Statistical analysis: All the data obtained were presented in percentages and frequencies using Microsoft excel.
Results: Out of 446 urine samples, 139 children were positive for pathogenic organisms. Escherichia coli constituted for 118 (84%) organisms followed by Proteus Mb 12 (8.6%) and Klebsiella sp 9 (6.4%).The organisms were found to be most sensitive to Amikacin (98%), Gentamicin (66%), and Ofloxacin (55%.).
Conclusion: E.coli is the leading pathogen causing UTI in children. It is highly sensitive to amikacin and is resistant to most of the commonly used antibiotics. This knowledge is necessary to treat UTI empirically in the local population.
Downloads
References
Kashef N, Djavid GE, Shahbazi S. Antimicrobial susceptibility patterns of community- acquired uropathogens in Tehran, Iran. J Infect Dev Ctries. 2010;(4):202–206. doi: https://doi.org/10.3855/jidc.540.
May OW. Urine Collection Methods in Children. Nur Clin North Am. 2018;53(2):137–143. doi: https://doi.org/10.1016/j.cnur.2018.01.001.
Shaikh N, Morone NE, Bost JE, Farrell MH. Prevalence of urinary tract infection in childhood: a meta-analysis. Pediatr Infect Dis J. 2008;27(4):302-308. doi: https://doi.org/10.1097/inf.0b013e31815e4122.
Muoneke V, Ibekwe M, Ibekwe R. Childhood urinary tract infection in abakaliki: etiological organisms and antibiotic sensitivity pattern. Ann Med Health Sci Res. 2012;2(1):29-32. doi: https://doi.org/10.4103/2141-9248.96933..
Marol R, Marol R, Marol R. Prevalence of urinary tract infection in febrile infants. Indian J Child Health. 2020; 7(2):85-88.
Kibar Y. Current Management of Urinary Tract Infection in Children. Urinary Tract Infections. 2011 Oct 3:267.
Chang SL, Shortliffe LD. Pediatric urinary tract infections. Pediatr Clin North Am. 2006;53(3):379-400. doi: https://doi.org/10.1016/j.pcl.2006.02.011.
Catal F, Bavbek N, Bayrak O, Karabel M, Karabel D, Odemis E, Uz E. Antimicrobial resistance patterns of urinary tract pathogens and rationale for empirical therapy in Turkish children for the years 2000–2006. Int Urol Nephrol. 2009;41(4):953. doi: https://doi.org/10.1007/s11255-008-9445-5.
Balasubramanian S, Kuppuswamy D, Padmanabhan S, Chandramohan V, Amperayani S. Extended-spectrum beta-lactamase-producing community-acquired urinary tract infections in children: Chart review of risk factors. J Glob Infect Dis. 2018;10(4):222-225. doi: https://dx.doi.org/10.4103%2F0974-777X.246391.
Kalaitzidou I, Ladomenou F, Athanasopoulos E, Anatoliotaki M, Vlachaki G. Susceptibility patterns of uropathogens identified in hospitalized children. Pediatr Int. 2019;61(3):246-251.doi:https://doi.org/10.1111/ped.13772.
Madhi F, Jung C, Timsit S, Levy C, Biscardi S, Lorrot M, et al. Febrile urinary-tract infection due to extended-spectrum beta-lactamase–producing Enterobacteriaceae in children: A French prospective multicenter study. PloS one. 2018;13(1):e0190910. doi: https://doi.org/10.1371/journal.pone.0190910.
Taneja N, Chatterjee SS, Singh M, Singh S, Sharma M. Pediatric urinary tract infections in a tertiary care center from north India. Indian J Med Res. 2010;131(1):101-106.
Pouladfar G, Basiratnia M, Anvarinejad M, Abbasi P, Amirmoezi F, Zare S. The antibiotic susceptibility patterns of uropathogens among children with urinary tract infection in Shiraz. Med. 2017;96(37):e7834. doi: https://doi.org/10.1097/md.0000000000007834.
Hameed T, Al Nafeesah A, Chishti S, Al Shaalan M, Al Fakeeh K. Community-acquired urinary tract infections in children: Resistance patterns of uropathogens in a tertiary care center in Saudi Arabia. Int J Pediatr Adolesc Med.2019 Jun;6(2):51-54. doi: https://doi.org/10.1016/j.ijpam.2019.02.010.
Badhan R, Singh DV, Badhan LR, Kaur A. Evaluation of bacteriological profile and antibiotic sensitivity patterns in children with urinary tract infection: A prospective study from a tertiary care center. Indian J Urol. 2016;32(1):50-56. Available from: http://www.indianjurol.com/text.asp?2016/32/1/50/173118.
Mitiku E, Amsalu A, Tadesse BT. Pediatric urinary tract infection as a cause of outpatient clinic visits in Southern Ethiopia: A cross sectional study. Ethiop J Health Sci 2018;28(2):187-196. doi: https://dx.doi.org/10.4314%2Fejhs.v28i2.10.
Vijayakumar M, Kanitkar M, Nammalwar BR, Bagga A. Revised statement on management of urinary tract infections. Indian Pediatr. 2011;48(9):709-717.
Tosif S, Baker A, Oakley E, Donath S, Babl FE. Contamination rates of different urine collection methods for the diagnosis of urinary tract infections in young children: An observational cohort study. J Paediatr Child Health 2012;48(8):659-664. doi: https://doi.org/10.1111/j.1440-1754.2012.02449.x.
Habte TM, Dube S, Ismail N, Hoosen AA. Hospital and community isolates of uropathogens at a tertiary hospital in South Africa. S Afr Med J 2009;99(8):584-587.
Sriram G,Satyanarayana A, Naik DR, Chandra TJ. Prevalence of urinary tract infection in febrile children between one to five years of age. Pediatric Rev: IntJPediatri Res. 2019;6(10):542-546. Available from: https://pediatrics.medresearch.in/index.php/ijpr/article/view/537.
Kwan CW, Onyett H. Community-acquired urinary tract pathogens and their resistancepatterns in hospitalized children in South Eastern Ontario between 2002 and 2008.Paediatr Child Health. 2008;13(9):759-762. doi: https://doi.org/10.1093/pch/13.9.759.
Sharifian M, Karimi A, Tabatabaei SR, Anvaripour N. Microbial sensitivity pattern in urinary tractinfections in children: a single center experience of 1, 177 urine cultures. Jpn J Infect Dis. 2006;59(6):380-382.
Amin EK, Abo Zaid AM, I Kotb AER, El-Gamasy MA. Incidence, risk factors and causative bacteria of urinary tract infections and their antimicrobial sensitivity patterns in toddlers and children: A report from two tertiary care hospitals.SaudiKidneyDisTranspl. 2020;31(1):200-208. doi: https://doi.org/10.4103/1319-2442.279941.
Mamuye Y. Antibiotic Resistance Patterns of Common Gram-negative Uropathogens inSt. Paul's Hospital Millennium Medical College. Ethiop J Health Sci. 2016; 26(2):93-100. doi: https://doi.org/10.4314/ejhs.v26i2.2.
Prajapati BS, Prajapati RB, Patel PS. Advances in management of urinary tractinfections. Indian J Pediatr. 2008;75(8):809–814.
Akram M, Shahid M, Khan AU. Etiology and antibiotic resistance patterns of community-acquired urinary tract infections in JNMC Hospital Aligarh, India. Ann Clin Microbiol antimicrob. 2007;6(1):4. doi: https://doi.org/10.1186/1476-0711-6-4.
Rai GK, Upreti HC, Rai SK, Shah KP, Shrestha RM. Causative agents of urinary tract infections in children and their antibiotic sensitivity pattern: a hospital based study. Nepal Med Coll J. 2008;10(2):86-90.
Kalantar E, Motlagh ME, Lornejad H, Reshadmanesh N. Prevalence of urinary tractpathogens and antimicrobial susceptibility patterns in children at hospitals in Iran.Iran J Clin Infect Dis. 2008;3:149-153.
Mashouf RY, Babalhavaeji H, Yousef J. Urinary tract infections: Bacteriology and antibiotic resistance patterns. Indian Pediatr. 2009;46(7):617-620.
Brad GF, Sabau I, Marcovici T, Maris I, Daescu C, Belei O, et al. Antibiotic resistance in urinary tract infections in children. J Pediatr 2010;13 (51-52):73-77.
Gupta V, Yadav A, Joshi RM. Antibiotic resistance pattern in uropathogens. Indian J Med Microbiol. 2002;20(2):96-98.Available from: http://www.ijmm.org/text.asp?2002/20/2/96/8358.
Moore CE, Sona S, Poda S, Putchhat H, Kumar V, Sopheary S, Stoesser N, Bousfield R, Day N, Parry CM. Antimicrobial susceptibility of uropathogens isolated from Cambodian children. Paediatr Int Child Health. 2016;36(2):113-117. doi: https://doi.org/10.1179/2046905515y.0000000008.
Akhtar MS, Mohsin N, Zahak A, Ain MR, Pillai PK, Kapur P, et al. Antimicrobial sensitivity pattern of bacterial pathogens in urinary tract infections in South Delhi, India. Rev Recent Clin Trials. 2014;9(4):271-275. doi: https://doi.org/10.2174/1574887109666141127104220.
Afsharpaiman S, Bairaghdar F, Torkaman M, Kavehmanesh Z, Amirsalari S, Moradi M. Bacterial pathogens and resistance patterns in children with community-acquired urinary tract infection: a cross sectional study. J Compre Pediat. 2012;3(1):16-20. doi: http://dx.doi.org/10.17795/compreped-7078.
Priyadharshana U, Piyasiri LB, Wijesinghe CPrevalence. antibiotic sensitivity pattern and genetic analysis of extended spectrum beta lactamase producing Escherichia coli and Klebsiella spp among patients with community acquired urinary tract infection in Galle district. Sri Lanka Ceylon Med J. 2019;64(4):140-145. doi: https://doi.org/10.4038/cmj.v64i4.8990.
Kothari A, Sagar V. Antibiotic resistance in pathogens causing community-acquired urinary tract infections in India: A multicenter study. J Infect Dev Ctries. 2008;2(5):354-358. doi: https://doi.org/10.3855/jidc.196.
Niranjan V, Malini A. Antimicrobial resistance pattern in Escherichia coli causing urinary tract infection among inpatients. Indian J Med Res. 2014;139(6):945-948.
Yildiz B, Kural N, Durmaz G, Yarar C, Ak I, Akcar N. Antibiotic resistance in children with complicated urinary tract infection. Saudi Med J. 2007;28(12):1850-1854.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


