To study the short term outcome and risk factors for premature neonate born at Dr. Bhimrao Ambedkar Memorial Hospital, Raipur, CG
Abstract
Background: Prematurity is the leading cause of perinatal morbidity and mortality worldwide,23 affecting 5-10% of births. Preterm neonates have a 120 times higher risk of death than neonates. The prevention of premature birth is the single most important challenge to modern obstetrics today. Progress in this area has been hampered by lack of understanding of the basic mechanisms responsible for premature labour and delivery. Thus, the following is a study on the short term outcomes and risk factors of preterm babies born at Dr B R Ambedkar Memorial hospital, conducted to evaluate the early outcomes of premature infants at the time of discharge and the identification of different risk factors for preterm births.
Methods: This is a prospective hospital based observational study, conducted over a period of 1 year (March 2018 – march 2019), including a total of 1472 preterm babies.
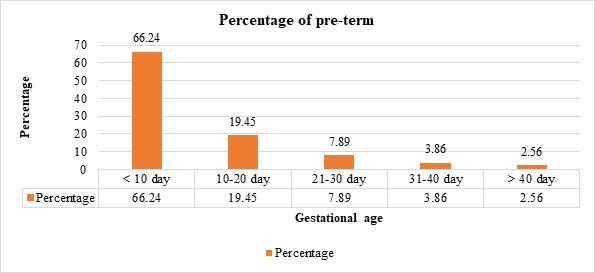
Results: A total of 1472 preterm were born during the study period. Preterm male: female was 1.1:1. Obstetrics history of mothers showed 47.35% were having parity-1, 30.71% were having parity-2. Common risk factors noted were multiple pregnancy (28.46%) followed by pre-eclampsia (27.03%). A total of 66.71% of neonates were born beyond 34 weeks of gestation, 60.46% were having birth weight between 1500 and 2499 gm, 18.14% were very low birth weight (VLBW) and 4.35% were extremely low birth weight (ELBW). A total of 545 (37.02%) required NICU admission. Major morbidities noted were respiratory distress syndrome (55.59%) followed by sepsis (30.64%), perinatal asphyxia (11.19%), neonatal jaundice (10.64%) and retinopathy of prematurity (9.91%). A negative correlation was noted between gestational age and duration of stay in NICU (r = 0.98, p = 0.022). Birth weight and gestational age of neonates were significantly associated with the treatment outcome(p=0.000). Very low birth weight neonates had highest mortality (40.85%) followed by ELBW (28.05%). Mortality of 11.14% was noted with respiratory distress syndrome (10.83%) being the major cause followed by sepsis (8.07%).
Conclusions: The most common maternal risk factors noted were multiple pregnancies, preeclampsia, eclampsia, antepartum haemorrhage and gestational hypertension. Common morbidities observed in preterm babies were respiratory distress syndrome, sepsis, perinatal-asphyxia and neonatal-jaundice. The common causes of death were respiratory distress syndrome, sepsis and prematurity. Results show that preterm babies have higher risk for morbidity and mortality. Mortality decreased with increase in gestational age and birth weight.
Downloads
References
Ahumada-Barrios ME, Alvarado GF. Fatores de Risco para partoprematuroem um hospital. Revista Latino-Americana de Enfermagem. 2016;24:e2750. doi: https://doi.org/10.1590/1518-8345.0775.2750.
Trønnes H, Wilcox AJ, Lie RT, Markestad T, Moster D. Risk of cerebral palsy in relation to pregnancy disorders and preterm birth: a national cohort study. Dev Med Child Neurol. 2014;56(8):779-785. doi: https://doi.org/10.1111/dmcn.12430.
Meza-Martínez J. Maternal factors related to the preterm term and its impact on the newborn. Hipólito National Hospital Nanue: 2002-2006. Peruvian Mag Obstet Nurs. 2007;19;3(2).
Lawn JE, Wilczynska-Ketende K, Cousens SN. Estimating the causes of 4 million neonatal deaths in the year 2000. Int JEpidemiol. 2006;35(3):706-718. doi: https://doi.org/10.1093/ije/dyl043.
Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. The Lancet. 2008;371(9606):75-84. doi: https://doi.org/10.1016/s0140-6736(08)60074-4.
Rees S, Inder T. Fetal and neonatal origins of altered brain development. Early Hum Dev. 2005;81(9):753-761. doi: https://doi.org/10.1016/j.earlhumdev.2005.07.004.
Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am JRespirCrit Care Med. 2001;163(7):1723-1729. doi: https://doi.org/10.1164/ajrccm.163.7.2011060.
Henderson JJ, McWilliam OA, Newnham JP, Pennell CE. Preterm birth aetiology 2004–2008. Maternal factors associated with three phenotypes: spontaneous preterm labour, preterm pre-labour rupture of membranes and medically indicated preterm birth. J MaternFetal Neonatal Med. 2012;25(6):642-647. doi: https://doi.org/10.3109/14767058.2011.597899.
Conde-Agudelo A, Rosas-Bermúdez A, Kafury-Goeta AC. Birth spacing and risk of adverse perinatal outcomes: a meta-analysis. JAMA. 2006;295(15):1809-1823. doi: https://doi.org/10. 1001/jama.295.15.1809.
Kramer MS, Demissie K, Yang H, Platt RW, Sauvé R, Liston R. Fetal and Infant Health Study Group of the Canadian Perinatal Surveillance System. The contribution of mild and moderate preterm birth to infant mortality. JAMA. 2000;284(7):843-889.https://doi.org/10.1001/jama.284.7.843.
Raju TN. The problem of late-preterm (near-term) births: a workshop summary. Pediatr Res. 2006;60(6):775-776. doi: https://doi.org/10.1203/01.pdr.0000246074.73342.1e
Wang ML, Dorer DJ, Fleming MP, Catlin EA. Clinical outcomes of near-term infants. Pediatr. 2004;114(2):372-376. doi: https://doi.org/10.1542/peds.114.2.372.
Kinney HC. The near-term (late preterm) human brain and risk for periventricular leukomalacia: a review. InSeminars in perinatology 2006, WB Saunders. Vol. 30, No. 2, pp. 81-88.
Escobar GJ, McCormick MC, Zupancic JA, Coleman-Phox K, Armstrong MA, Greene JD, et al. Unstudied infants: outcomes of moderately premature infants in the neonatal intensive care unit. ArchDis ChildFetal Neonatal Ed. 2006;91(4):F238-F244. doi: https://dx.doi.org/10.1136%2Fadc.2005.087031.
Roberts D, Brown J, Medley N, Dalziel SR. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 2017;3(3):CD004454. doi: https://doi.org/10.1002/14651858.cd004454.pub3.
Soll RF. Surfactant treatment of the very preterm infant. Neonatol. 1998;74(1):35-42. doi: https://doi.org/10.1159/000047033.
Gultom E, Doyle LW, Davis P, Dharmalingam A, Bowman E. Changes over time in attitudes to treatment and survival rate for extremely preterm infants (23–27 weeks' gestational age). Aust N Z JObstet Gynaecol. 1997;37(1):56-58. doi: https://doi.org/10.1111/j.1479-828x.1997.tb02218.x
Doyle LW, Rogerson S, Chuang SL, James M, Bowman ED, Davis PG. Why do preterm infants die in the 1990s. Med J Aust. 1999;170(11):528-532. doi: https://doi.org/10.5694/j.1326-5377.1999.tb127877.x.
Draper ES, Manktelow B, Field DJ, James D. Prediction of survival for preterm births by weight and gestational age: retrospective population-based study. BMJ. 1999;319(7217):1093-1097. doi: https://dx.doi.org/10.1136%2Fbmj.319.7217.1093.
Hagan R, Benninger H, Chiffings D, Evans S, French N. Very preterm birth–A regional study. Part 2: The very preterm infant. BJOG: Int J Obstet Gynaecol. 1996;103(3):239-245. doi: https://doi.org/10.1111/j.1471-0528.1996.tb09712.x.
Doyle LW. Outcome at 5 years of age of children 23 to 27 weeks' gestation: refining the prognosis. Pediatr. 2001;108(1):134-141. doi: https://doi.org/10.1542/peds.108.1.134.
Sugantha R, Nanthini N, Padmanaban S. Evaluation of nifedipine tocolysis in preterm labour.Int J Clin Obstet Gynaecol. 2019;3(2):76-78. doi: https://doi.org/10.33545/gynae.2019.v3.i2b.223.
Shiono PH, Klebanoff MA. Ethnic differences in preterm and very preterm delivery. Am J Public Health. 1986;76(11):1317-1321. doi: https://dx.doi.org/10.2105%2Fajph.76.11.1317.
Pickering RM, Deeks JJ. Risks of delivery during the 20th to the 36th week of gestation. Int JEpidemiol. 1991;20(2):456-466. doi: https://doi.org/10.1093/ije/20.2.456.
de Sanjose S, Roman E. Low birthweight, preterm, and small for gestational age babies in Scotland, 1981-1984. J Epidemiol Comm Health. 1991;45(3):207-210. doi: https://dx.doi.org/10.1136%2Fjech.45.3.207.
Papiernik E. The principal risk factors for preterm delivery. Effective prevention of preterm birth: the French experience measured at Haguenau. 1989:29-37.
Meyer MB, Jonas BS, Tonascia JA. Perinatal events associated with maternal smoking during pregnancy. Am J Epidemiol. 1976;103(5):464-476. doi: https://doi.org/10.1093/oxfordjournals.aje.a112248.
Mamelle N, Laumon B, Lazar P. Prematurity and occupational activity during pregnancy. Am JEpidemiol. 1984;119(3):309-322. doi: https://doi.org/10.1093/oxfordjournals.aje.a113750.
Rubaltelli FF, Bonafè L, Tangucci M, Spagnolo A, Dani C. Epidemiology of neonatal acute respiratory disorders. Neonatol. 1998;74(1):7-15. doi: https://doi.org/10.1159/000014005.
Bang AT, Reddy HM, Bang RA, Deshmukh MD. Why do neonates die in rural Gadchiroli, India?(Part II): estimating population attributable risks and contribution of multiple morbidities for identifying a strategy to prevent deaths. JPerinatol. 2005;25(1):S35-S43. doi: https://doi.org/10.1038/sj.jp.7211270.
Atasay B, Okulu E, MunganAkın İ, Çandır O, Arsan S, Türmen T. The early clinical outcomes of late preterm newborns. Turkish J Pediatric Dis. 2010;4:30-35.
Kalyoncu Ö, Aygün C, Çetİnoğlu E, Küçüködük S. Neonatal morbidity and mortality of late-preterm babies. J Mat-Fet Neonat Med. 2010;23(7):607-612. doi: https://doi.org/10.3109/14767050903229622.
Shrestha S, Dangol SS, Shrestha M, Shrestha RP. Outcome of preterm babies and associated risk factors in a hospital. J Nepal Med Assoc. 2010;50(180):286-290.
Marchant T, Willey B, Katz J, Clarke S, Kariuki S, Ter Kuile F, et al. Neonatal mortality risk associated with preterm birth in East Africa, adjusted by weight for gestational age: individual participant level meta-analysis. PLoS medicine. 2012;9(8):e1001292. doi: https://doi.org/10.1371/journal.pmed.1001292.
Iyoke CA, Lawani OL, Ezugwu EC, Ilechukwu G, Nkwo PO, Mba SG, et al. Prevalence and perinatal mortality associated with preterm births in a tertiary medical center in South East Nigeria. Int JWomen's Health. 2014;6:881-888. doi: https://doi.org/10.2147/ijwh.s72229.
Cupen K, Barran A, Singh V, Dialsingh I. Risk factors associated with preterm neonatal mortality: a case study using data from Mt. Hope Women’s Hospital in Trinidad and Tobago. Children. 2017;4(12):108. doi: https://doi.org/10.3390/children4120108.
Poudel P, Budhathoki S, Shrivastava MK. Maternal risk factors and morbidity pattern of very low birth weight infants: A NICU based study at eastern Nepal. J Nepal Paediatr Soc. 2009;29(2):59-66. doi: https://doi.org/10.3126/jnps.v29i2.2040.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


