Seronegative dengue cases in children – a retrospective analysis in a tertiary care center in Puducherry
Abstract
Objectives: This study was undertaken to know the clinical profile and outcome of seronegative dengue cases in children, admitted to a tertiary care teaching hospital in Puducherry.
Materials and methods: This is a hospital-based, retrospective, descriptive study, done on seronegative dengue cases, of children aged 1 to 15 years of age, admitted and treated in the pediatric department and pediatric intensive care unit from June 2017 - December 2019, in Sri Venkateshwaraa Medical College :and Research Centre, Puducherry.
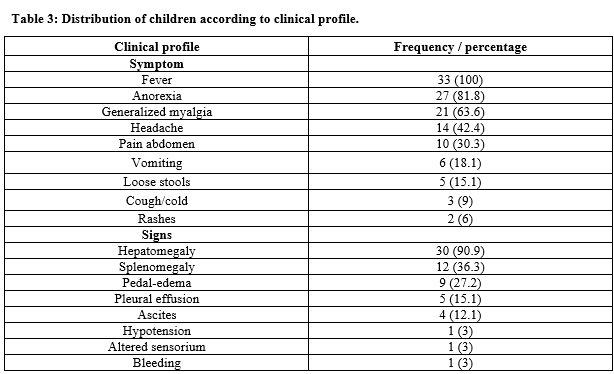
Results: About 75 children were suspected of dengue fever during the study period and those blood samples were sent for dengue serology. Only 16 cases (21.3%) were reported to be dengue serology positive. The remaining 59 (78.6%) were dengue serology negative. A total of about 33 children who fulfilled the inclusion criteria were studied and the results were analyzed. It was seen that, male children outnumbered (69.6%), females (30.3%). Maximum numbers of cases were seen among 11-15 years of age (51.5%), followed by (36.3%) in 6 to 10 years of age and (12.1%) in 1-5 years of age. The most common symptom at presentation was, fever seen in (100%) of cases, followed by anorexia in (81.8%), generalized myalgia (63.6%), headache (42.4%), pain abdomen (30.3%), vomiting in (18.1%). Rare symptoms were, loose stools in (15.1%), cough (9%), rashes (6%). The most common sign was hepatomegaly (90.9%), followed by splenomegaly (36.3%), pedal edema (27.2%), pleural effusion (15.1%), ascites (12.1%) and hypotension, altered sensorium and bleeding in (3%) of cases. It was seen that (63.6%) of patients were discharged in < 5 days, most of them belong to DF without warning signs. About (36.3%) were discharged after 5 days of admission; most of them had DF warning signs. According to the outcome, it was seen that (84.8%) were discharged, (2.1%) went against medical advice and (3%) of severe dengue was discharged at request.
Conclusion: The current study has revealed that seronegative dengue cases are more common than seropositive cases in children. They present with common symptoms and rarely atypical symptoms. Clinical diagnosis is more important because of the increasing trend of seronegative dengue cases in children, either because of late or atypical presentation and since the burden of dengue is being underestimated. A high index of clinical suspicion is needed, in spite of seronegativity in children with dengue, in order to reduce the morbidity and improve the outcome in epidemics as well as in daily clinical practice.
Downloads
References
World Health Organization. (2009). Dengue guidelines for diagnosis, treatment, prevention and control : new edition. World Health Organization. Available at https://apps.who.int/iris/handle/10665/44188.
Chaturvedi UC, Nagar R. Dengue and dengue haemorrhagic fever: Indian perspective. J Biosci. 2008;33(4):429-441. doi: https://doi.org/10.1007/s12038-008-0062-3.
Gubler DJ. Dengue/dengue haemorragic fever: history and current status. Novartis Found Symp. 2006;277:3-16. doi: https://doi.org/10.1002/0470058005.ch2.
Ratageri VH, Wari SP, Chavan SC, Mujahid IB, Yergolkar PN. Clinical Profile and Outcome of Dengue Fever Cases. Indian J Pediatr. 2005;72(8):705-706. doi: https://doi.org/10.1007/bf02724083.
Kadam DB, Salvi S, Chandanwale A. Expanded Dengue. J Assoc Physicians India. 2016;64(7):59-63.
Chacko B, Subramanian G. Clinical, Laboratory and Radiological Parameters in Children with Dengue Fever and Predictive Factors for Dengue Shock Syndrome. J Trop Pediatr. 2007;54(2):265-270. doi: https://doi.org/10.1093/tropej/fmm084.
Pone SM, Hokerberg YH, de Oliveira RV, Daumas RP, Pone TM, Pone MV, et al. Clinical and laboratory signs associated with serious dengue disease in hospitalized children. J Pediatr (Rio J).2016;92(5):464-471. doi: https://doi.org/10.1016/j.jped.2015.12.005.
Padhi S, Dash M, Panda P, Parida B, Mohanty I, Sahu S, et al. A three-year retrospective study on the increasing trend in seroprevalence of dengue infection from southern Odisha, India. Indian J Med Res. 2014;140(5):660-664.
Chen Li C, Ho Chen C. Clinical features and dynamic ordinary laboratory tests differentiating dengue fever from other febrile illnesses in children. J Microbiol, Immunol Infect.2018;51(5);614-620. doi: https://doi.org/10.1016/j.jmii.2016.08.018
Narayanan M, Aravind N, Thilothammal R, Prema R, Sargunam CS, Ramamurty N. Dengue Fever Epidemic in Chennai–A Study of Clinical profile and Outcome. Indian Pediatr. 2002;39(11):1027-1033.
Malavige GN, Fernando S, Fernando DJ, Seneviratne SL. Dengue viral infections. Postgrad Med J. 2004;80(948):588-601. doi: https://doi.org/10.1136/pgmj.2004.019638.
Pothapregada S, Kamalakannan B, Thulasingham M, Sampath S. Clinical Profiling Pediatric Patients with Dengue. J Glob Infect Dis. 2016:8(3):115-120. doi: https://doi.org/10.4103/0974-777x.188596.
Mallhi TH, Khan AH, Adnan AS, Sarriff A, Khan YH, Jummaat F. Clinicolaboratory spectrum of dengue viral infection and risk feactors associated with dengue hemorrhagic fever :a retrospective study. BMC Infect Dis. 2015;15:399. doi: https://doi.org/10.1186/s12879-015-1141-3.
Pothapregada S, Kamalakannan B, Thulasingam M. Risk factors for shock in children with dengue fever. Indian J Crit Med. 2015;19(11):661-664. doi: https://doi.org/10.4103/0972-5229.169340.
Shah I, Deshpande GC, Tardeja PN. Outbreak of dengue in Mumbai and predictive markers for dengue shock syndrome. J Trop Pediatr. 2004;50(5):301-305. doi: https://doi.org/10.1093/tropej/50.5.301.
Propregada S, Kamalakannan B, Thulasingam M. Clinical profile of atypical manifestations of dengue fever. Indian J Pediatr. 2016;83(6):493-499. doi: https://doi.org/10.1007/s12098-015-1942-9.
Aggarwal A, Chandra J, Aneja S, Patwari AK, Dutta AK. An epidemic of dengue hemorrhagic fever and dengue shock syndrome in children in Delhi. Indian Pediatr. 1998;35(8):727-732.
Varatharaj A. Encephalitis in the clinical spectrum of dengue infection. Neurol India. 2010;58(4):585-591. doi: https://doi.org/10.4103/0028-3886.68655.
Mittal H, Faridi MMA, Arora SK, Patil R. Clinico hematological Profile and Platelet trends in Children with Dengue During 2010 Epidemic in North India. Indian J Pediatr 2012;79(4):467-471. doi: https://doi.org/10.1007/s12098-011-0586-7.
Mishra S, Ramanathan R, Agarwalla SK. Clinical Profile of Dengue Fever in Children : A Study from Southern Odisha, India. Scientifica 2016;2016:6391594. doi: https://dx.doi.org/10.1155%2F2016%2F6391594.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


