Maternal Risk factors, morbidity, and mortality pattern of LBW babies admitted in NICU: A Retrospective study done in Banas Medical College and Research Centre, Palanpur, Gujarat, India
Abstract
Background: This study was undertaken to know about the maternal risk factors, morbidity, and mortality of low birth weight (LBW) babies admitted to NICU in a tertiary care hospital.
Methods: This is a hospital-based, retrospective, descriptive study, done on LBW babies admitted to the NICU of Banas Medical College and Research Institute, Palanpur from January 2019- March 2020.
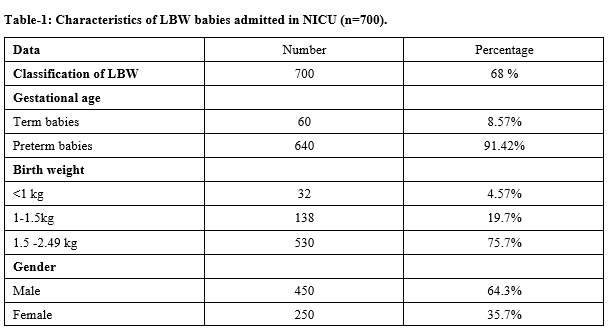
Results: Out of the 1018 newborns admitted to NICU, 735 were LBW babies and 700 LBW babies were analyzed because 35 cases did not fit in inclusion criteria. The magnitude of LBW babies was 68.7 %.Out of 700 LBW babies, 530 (75.7%) had weight between 1.5kg to 2.49 kg,138 (19.7%) babies were of VLBW ( 1kg -1.5kg) and 32(4.57%) babies were of ELBW (weight <1 kg).Out of 700 LBW babies, 450 (64.3%)were males and 250(35.7%) were females and 60 (8.57%) were term babies and 640 (91.42%)were preterm babies. Among the maternal risk factors most common was maternal undernutrition (30%), followed by maternal anemia in 180 cases (25.7%), inadequate ANC visits in 170 cases (24.2%), maternal age <20 years in 110 cases (15.7%). Less common causes were bad obstetric history (1.14%), Twins delivery (1%), acute infections, and elderly primi (0.85%) respectively and the least common was PROM in 0.42%. Out of 700 babies, morbidity was seen in 590 LBW babies (84.28%).
Conclusion: Identification of maternal risk factors and providing proper care and appropriate management to LBW can reduce neonatal morbidity and mortality
Downloads
References
Roudbari M, Yaghmaei M, Soheili M. Prevalence, and risk factors of low-birth-weight infants in Zahedan, Islamic Republic of Iran. EMHJ-Eastern Mediterr Health J. 2007;13(4):838-845.
Behrman RE, Kliegman RM, eds. Nelson essentials of pediatrics. 4th ed; Philadelphia, WB Saunders, 2002.
McCormick MC. The contribution of low birth weight to infant mortality and childhood morbidity. New Eng J Med. 1985;312(2):82-90.
Stoll BJ, Kliegman RM, High risk infant: In: Behrman RE, Kliegman RM, Jenson HB, editors Nelson textbook of Paediatrics. 17th Edition; Philadelphia: Saunders;2004:547-559.
Villar J, Belizán J. The relative contribution of prematurity and fetal growth retardation to low birth weight in developing and developed societies. Am J Obstet Gynecol. 1982;143(7):793-798.
Klingenberg C, Olomi R, Oneko M, Sam N, Langeland N. Neonatal morbidity and mortality in a Tanzanian tertiary care referral hospital. Annals Trop Paediatr. 2003;23(4):293-299. doi: 10.1179/027249303225007806.
Kusin JA, Kardjati S, Renqvist UH. Maternal body mass index: the functional significance during reproduction. Europe J Clin Nutri. 1994.
Bang AT, Bang RA, Baitule SB, Reddy MH, Deshmukh MD. Effect of home-based neonatal care and management of sepsis on neonatal mortality: field trial in rural India. Lancet. 1999;354(9194):1955-1961. doi: 10.1016/S0140-6736(99)03046-9.
UNAIDS. AIDS epidemic update: Geneva: United Nations Administrative Committee on Coordination Sub Committee on Nutrition (2000). Low Birth Weight: Nutrition Policy Paper No 18.
Verma V, Das KB. Teenage primigravidae: a comparative study. Indian J Public Health. 1997;41(2):52-55.
McIntrire DD, Bloom SL, Casey BM, Leveno KJ. Birth weight in relation to morbidity and mortality among new born infants. N Engl J Med 1999;340(16):1234-1238. doi: 10.1056/NEJM199904223401603.
Parikh T, Parikh A, Maternal risk factors and outcome of low birth weight babies admitted to a Gujarat Adani Institute of Medical Science, Bhuj, Kutch, Gujarat, India- A cross-sectional study. Int J Med Paediatr Oncol. 2017:3(2):54-56. doi: 10.18231/2455-6793.2017.0015.
Deswal BS, Singh JV, Kumar D. A study of Risk factors for low birth weight. Indian J Comm Med. 1999;24(3):127-131.
Mannan MA, Jahan N, Dey SK, Uddin MF, Ahmed S. Maternal and foetal risk factor and complication with immediate outcome during hospital stay of very low birth weight babies. Mymensingh Med J: MMJ. 2012;21(4):639.
Naskar N, Swain A, Das KN, Patnayak AB. Maternal risk factors, complications and outcome of very low birth weight babies: prospective cohort study from a tertiary care centre in Odisha. J Neonatal Biol. 2014;3:2167-0897. doi: 10.4172/2167-0897.1000142.
Manganaro R, Gemelli M, Mami C, Mancuso A, Rizza ML, Leonardi R. Analysis of factors associated with very low birth weight (less than or equal to 1500 g). Minerva ginecologica. 1991;43(6):283-286.
Roy KK, Baruah J, Kumar S, Malhotra N, Deorari AK, Sharma JB. Maternal antenatal profile and immediate neonatal outcome in VLBW and ELBW babies. Indian J Pediatr. 2006;73(8):669. doi: 10.1007/BF02898441.
Scholl TO., Johnson WG. Folic acid influence on the outcome of pregnancy. Am J Clin Nutri. 2000;71(5):1295S-1303S. doi: 10.1093/ajcn/71.5.1295.
Chidiebere ODI, Uchenna E, Ikenna KN, Christian I, Nwabueze AI, Ogechukwu FA. The Low-birth weight Infants: Pattern of Morbidity and Mortality in a tertiary Health care Facility in the South Eastern Nigeria. Ann Med Health Sci Res. 2018;8:4-10.
Steer PJ. Maternal hemoglobin concentration and birth weight. Am J Clin Nutri. 2000;71(5):1285S-1287S. doi: 10.1093/ajcn/71.5.1285s.
Ronnenberg AG, Wood RJ, Wang X, Xing H, Chen C, et al. Preconception hemoglobin and ferritin concentrations are associated with pregnancy outcome in a prospective cohort of Chinese women. J Nutri. 2004,134(10):2586-2591. doi: 10.1093/jn/134.10.2586.
Poudel P, Budhathoki S, Shrivastava MK. Maternal risk factors and morbidity pattern of very low birth weight infants: A NICU based study at eastern Nepal. J Nepal Paediatr Soc. 2009;29(2):59-66. doi: 10.3126/jnps.v29i2.2040.
Tagare A, Chaudhari S, Kadam S, Vaidya U, Pandit A, Sayyad MG. Mortality and morbidity in extremely low birth weight (ELBW) infants in a neonatal intensive care unit. Indian J Pediatr. 2013;80(1):16-20. doi:10.1007/s12098-012-0818-5.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


