Benefits of 100% human milk diet in preterm infants: NICU Nurses Survey
Abstract
Background: Hundred percent human milk diet plays a vital part in the nutritional management of preterm infants in the Neonatal Intensive Care Unit (NICU). NICU nurses play an important role in the management of nutrition and growth of preterm infants, who will also oversee the implementation of an exclusive human milk diet (EHMD) in the NICU.
Objective: To understand the NICU nurses' perspectives on the benefits of 100% human milk diet through human milk-derived nutritional products in preterm infants.
Material and Methods: Online survey was conducted through Google Forms which had nine questions on the benefits of human milk-based nutrition finalized by expert neonatologists. An online survey link was shared with the NICU nurses through emails and text messages. A request was made to the neonatologists and head nurses to disseminate the survey link with their counterparts and colleagues.
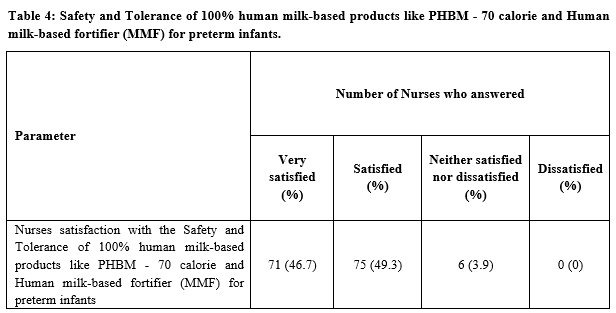
Results: All the participants rated that exclusive breastfeeding or using 100% Human Milk Diet is very important for preterm babies in NICU [n=152 (100%)]. 46.7% (n=71) participants reported that seventy calories pasteurized human breast milk, (PHBM – 70 Cal) is the best option for preterm infants when the mother’s own milk (MOM) is unavailable. 84.9% (n=129) of the participants stated that the Human milk-based fortifier (HMDF) – Mother’s Milk Fortifier (MMF) is the best option for fortification. 96% (n=146) participants were satisfied with the safety and tolerance of 100% human milk-based products like PHBM - 70 calories and MMF.
Conclusion: The majority of the NICU nurses in India are aware of the benefits of human milk and 100% human milk diet in preterm infants. Human milk-derived nutritional products; HMDF (MMF) and 70 Calories are reported to be having good tolerance and safety in preterm infants by most of the NICU nurses. Having regular training sessions about EHMD for NICU nurses would be impactful.
Downloads
References
Dicky O, Ehlinger V, Montjaux N, Gremmo‐Féger G, Sizun J, Rozé JC, et al. Policy of feeding very preterm infants with their mother's own fresh expressed milk was associated with a reduced risk of bronchopulmonary dysplasia. Acta Paediatr. 2017;106(5):755-762. doi: 10.1111/apa.13757.
Poindexter B. The direct and indirect influence of own mother's milk on bronchopulmonary dysplasia and costs. Arch Dis Child Fetal Neonatal Ed. 2017;102(3):F192-F193. doi: 10.1136/archdischild-2016-312197.
Patel AL, Johnson TJ, Robin B, Bigger HR, Buchanan A, Christian E, et al. Influence of own mother's milk on bronchopulmonary dysplasia and costs. Arch Dis Child Fetal Neonatal Ed. 2017;102(3):F256-F261. doi: 10.1136/archdischild-2016-310898.
Viswanathan S, Merheb R, Wen X, Collin M, Groh-Wargo S. Standardized slow enteral feeding protocol reduces necrotizing enterocolitis in micropremies. J Neonatal Perinatal Med. 2017;10(2):171-180. doi: 10.3233/NPM-171680.
Cacho NT, Parker LA, Neu J. Necrotizing Enterocolitis and Human Milk Feeding: A Systematic Review. Clin Perinatol. 2017;44(1):49-67. doi: 10.1016/j.clp.2016.11.009.
Maffei D, Schanler RJ. Human milk is the feeding strategy to prevent necrotizing enterocolitis!. Semin Perinatol. 2017;41(1):36-40. doi: 10.1053/j.semperi.2016.09.016.
Perrine CG, Scanlon KS. Prevalence of use of human milk in US advanced care neonatal units. Pediatrics. 2013;131(6):1066-1071. doi: 10.1542/peds.2012-3823.
Cristofalo EA, Schanler RJ, Blanco CL, Sullivan S, Trawoeger R, Kiechl-Kohlendorfer U, et al. Randomized trial of exclusive human milk versus preterm formula diets in extremely premature infants. J Pediatr. 2013;163(6):1592-1595. doi: 10.1016/j.jpeds.2013.07.011.
Sullivan S, Schanler RJ, Kim JH, Patel AL, Trawöger R, Kiechl-Kohlendorfer U, et al. An exclusively human milk-based diet is associated with a lower rate of necrotizing enterocolitis than a diet of human milk and bovine milk-based products. J Pediatr. 2010;156(4):562-567.e1. doi: 10.1016/j.jpeds.2009.10.040.
Abrams SA, Schanler RJ, Lee ML, Rechtman DJ, Prolacta Study Group. Greater mortality and morbidity in extremely preterm infants fed a diet containing cow Milk protein products. Breastfeed Med. 2014;9(6):281-285. doi: 10.1089/bfm.2014.0024.
Spatz DL, Edwards TM. The Use of Human Milk and Breastfeeding in the Neonatal Intensive Care Unit: Position Statement 3065. Adv Neonatal Care. 2016;16(4):254. doi:10.1097/ANC.0000000000000313
Hallowell SG, Spatz DL, Hanlon AL, Rogowski JA, Lake ET. Characteristics of the NICU work environment associated with breastfeeding support. Adv Neonatal Care. 2014;14(4):290-300. doi:10.1097/ANC.0000000000000102
Hair AB, Hawthorne KM, Chetta KE, Abrams SA. Human milk feeding supports adequate growth in infants £1250 grams birth weight. BMC Res Notes. 2013;6(1):459. doi:10.1186/1756-0500-6-459.
Dunn L, Hulman S, Weiner J, Kliegman R. Beneficial effects of early hypocaloric enteral feeding on neonatal gastrointestinal function. Preliminary report of a randomized trial. J Pediatr. 1988;112(4):622-629. doi:10.1016/s0022-3476(88)80185-9.
Slagle Ta, Gross SJ. Effect of early low volume enteral substrate on subsequent feeding tolerance in very low birth weight infants. J Pediatr. 1988;113(3):526-531. doi: 10.1016/s0022-3476(88)80646-2.
Berseth CL. Effect of early feeding on maturation of the preterm infants’ small intestine. J Pediatr. 1992;120(6):947-953. doi: 10.1016/s0022-3476(05)81969-9.
Tyson JE, Kennedy KA. Trophic feedings for parenterally fed infants. Cochrane Database Syst Rev. 2005;(3):CD000504. doi: 10.1002/14651858.CD000504.pub2.
Troche B, Harvey-Wilkes K, Engle WD, Nielsen HC, Frantz ID, Mitchell ML, et al. Early minimal feedings promote growth in critically ill premature infants. Biol Neonate. 1995;67(3):172-181. doi: 10.1159/000244160.
WHO. Every Newborn: An Action Plan to End Preventable Deaths. Geneva: World Health Organization, 2014. Available from: https://apps.who.int/iris/bitstream/handle/10665/127938/9789241507448_eng.pdf;jsessionid =C3B6F4BB283F8EA1A4606F4EE228CB21?sequence=1. Accessed May 8, 2020.
Committee on Nutrition, Section on Breastfeeding, Committee on Fetus and Newborn. Donor human milk for the high-risk infant: Preparation, safety, and usage options in the United States. Pediatr. 2017;139(1):e20163440. doi: 10.1542/peds.2016-3440.
Arslanoglu S, Corpeleijn W, Moro G, Braegger C, Campoy C, Colomb V, et al. Donor human milk for preterm infants: Current evidence and research directions. J Pediatr Gastroenterol Nutr. 2013;57(4):535-542. doi: 10.1097/MPG.0b013e3182a3af0a.
Sachdeva RC, Mondkar J, Shanbhag S, Sinha MM, Khan A, Dasgupta R. Landscape Analysis of Human Milk Banks in India. Indian Pediatr. 2019;56(8):663‐668.
Gidrewicz DA, Fenton TR. A systematic review and meta-analysis of the nutrient content of preterm and term breast milk. BMC Pediatr. 2014;14:216. doi: 10.1186/1471-2431-14-216.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


