Assessment of parents’ understanding of pediatric medical prescriptions
Abstract
Objective: To assess the accuracy of the parent understanding of pediatric prescription and prescribed medications and examine factors associated.
Methods: Cross-sectional, observational questionnaire-based study involving 354 eligible parents was carried out in the pediatric department of a tertiary care teaching hospital. Parent's sociodemographic details and their understanding of prescription including medication name, indication, dose, frequency, and duration were assessed by a self-administered questionnaire and their association analyzed statistically.
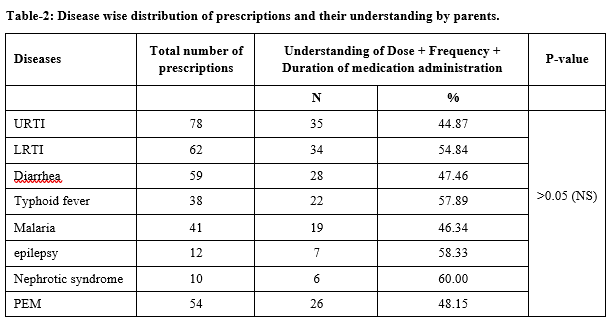
Results: Mean age of parents was 33 ± 1.2 with the majority of females 57.06%. Out of 354 parents, 22.32% had low literacy and 37.74% were working as farmers. Overall understanding of prescription was present in only 25.14% of parents. The majority of parents were having a better understanding of the frequency of drug administration (79.09), while poor understanding was observed with respect to dosage calculation of medication (45.76%) and adverse drug reactions (25.14%) and the difference in the understanding was statistically significant (P<0.05). Factors like the age of parents, Child’s age, parent occupation, education of parent, experience in administering medicine, number of medicines prescribed, and type of dosage form were significantly impacting parent’s understanding regarding medication (P<0.05).
Conclusion: Unperceived medication instruction understanding gaps exist at all literacy levels for pediatric patients among all parents. Communication and care delivery practices need further evaluation.
Practice implications: Clinicians should be aware of the frequency of parent medication misunderstanding and give more attention to parents’ counseling.
Downloads
References
Webb J, Davis TC, Bernadella P, Clayman ML, Parker RM, Adler D, et al. Patient-centered approach for improving prescription drug warning labels. Patient Educ Couns. 2008;72(3):443-449.
Wolf MS, Davis TC, Shrank WH, Neuberger M, Parker RM. A critical review of FDA-approved medication guides. Patient Educ Couns. 2006;62(3):316-322.
Wolf MS, Shekelle P, Choudhry NK, Agnew-Blais J, Parker RM, Shrank WH. Variability in pharmacy interpretations of physician prescriptions. Med Care.2009;47(3):370-373.
Holloway K, Van Dijk L. The world medicines situation 2011. Rational use of medicines. Geneva: WHO. 2011.
Kaushal R, Goldmann DA, Keohane CA, Christino M, Honour M, Hale AS, et al. Adverse drug events in pediatric outpatients. Ambulat Pediatr. 2007;7(5):383-389.
Kaufmann J, Laschat M, Wappler F. Medication Errors in Pediatric Emergencies. Dtsch Arztebl Int. 2012;109(38):609-616.
Wolf MS, Davis TC, Shrank W, Rapp DN, Bass PF, Connor UM, et al. To err is human: patient misinterpretations of prescription drug label instructions. Patient Educat Counsel. 2007;67(3):293-300.
Scherer YK, Bruce S. Knowledge, attitudes, and self-efficacy and compliance with medical regimen, number of emergency department visits, and hospitalizations in adults with asthma. Heart Lung. 2001;30(4):250-257.
Ogedegbe G, Mancuso CA, Allegrante JP, Charlson ME. Development and evaluation of a medication adherence self-efficacy scale in hypertensive African-American patients. J Clin Epidemiol. 2003;56(6):520-529.
Fernandez S, Chaplin W, Schoenthaler AM, Ogedegbe G. Revision and validation of the medication adherence self-efficacy scale (MASES) in hypertensive African Americans. J Behav Med. 2008;31(6):453-462.
Horan ML, Kim KK, Gendler P, Froman RD, Patel MD. Development and evaluation of the osteoporosis self-efficacy scale. Res Nurs Health. 1998;21(5):395-403.
Lorig K, Chastain RL, Ung E, Shoor S, Holman HR. Development and evaluation of a scale to measure perceived self-efficacy in people with arthritis. Arthritis Rheum.1989;32(1):37-44.
Resnick B, Wehren L, Orwig D. Reliability and validity of the self-efficacy and outcome expectations for osteoporosis medication adherence scales. Orthop Nurs.2003;22(2):139-147.
Ryu GS, Lee YJ. Analysis of liquid medication dose errors made by patients and caregivers using alternative measuring devices. J Manag Care Pharm. 2012;18(6):439-445.
Adams LV, Craig SR, Mmbaga EJ, Naburi H, Lahey T, Nutt CT, et al. Children's medicines in Tanzania: A national survey of administration practices and preferences. PLoS One. 2013;8(3):e58303.
Yin HS, Dreyer BP, Foltin G, van Schaick L, Mendelsohn AL. Association of low caregiver health literacy with reported use of nonstandardized dosing instruments and lack of knowledge of weight-based dosing. Ambul Pediatr. 2007;7(4):292-298.
Kendrick JG, Ma K, Dezorzi P, Hamilton D. Vomiting of oral medications by pediatric patients: Survey of medication redosing practices. Can J Hosp Pharm. 2012;65(3):196-201.
Wong IC, Wong LY, Cranswick NE. Minimising medication errors in children. Arch Dis Child. 2009;94(2):161-164.
Madlon-Kay DJ, Mosch FS. Liquid medication dosing errors. J Fam Pract. 2000;49(8):741-744.
McD Taylor D, Robinson J, MacLeod D, MacBean CE, Braitberg G. Therapeutic errors among children in the community setting: Nature, causes and outcomes. J Paediatr Child Health. 2009;45(5):304-309.
Glick AF, Farkas JS, Nicholson J, Dreyer BP, Fears M, Bandera C, et al. Parental management of discharge instructions: a systematic review. Pediatr. 2017;140(2):e20164165.
Al-Harthy N, Sudersanadas KM, Al-Mutairi M, Vasudevan S, Saleh GB, Al-Mutairi M, et al. Efficacy of patient discharge instructions: a pointer toward caregiver friendly communication methods from pediatric emergency personnel. J Family Community Med. 2016;23(3):155-160.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


