A pattern of poisoning in children- an experience from a teaching hospital in southern India
Abstract
Introduction: Poisoning in children is an important Paediatric emergency and is a worldwide problem. It is a common and preventable cause of morbidity and mortality in children.
Objectives: The aim of this study was to determine the profile and outcome of children less than 13 years admitted to the Paediatric department presenting with acute poisoning at a Teaching district hospital in southern Karnataka.
Methods: Prospectively, 134 acute poisoning cases, admitted to Paediatric intensive care, SIMS Shivamogga from November 2018 to May 2019 were included in this study.
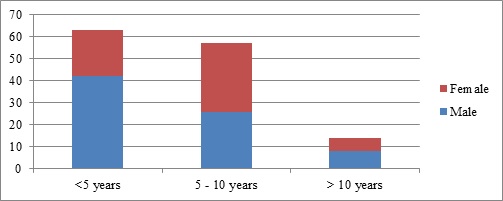
Results: During the study period, 134 patients presented with acute poisoning. The incidence of poisoning in Paediatric patients was 2.84%. The median age of our patients was 5.2 years (range 0.75-12 years). The male to female ratio was 1.58:1. Animal bites (27.61%), Petroleum products (26.87%), Household chemicals (15.67%), Drugs (11.19%), Poisonous plant derivatives (8.96%) and Insecticides (6.72%) were the agents most frequently implicated. Almost all (98.41%) cases in 1 to 5 years age group were accidental in nature, whereas in the >10 years age group, the majority (71.43%) were suicidal. Thirteen patients (9.7%) remained asymptomatic. The specific antidote was given to 19 (14.18%) patients. Three patients (2 snake bite and 1 rodenticide child) died. The mean duration of hospital stay was 4.49 days (range was 1 day to 22 days).
Conclusions: Accidental poisoning was common in children below 5 years of age. Minimal age of suicidal poisoning was 8 years. The most common agent implicated was a snake bite.
Downloads
References
Reddy KS, Murthy OP. The essential of forensic medicine and toxicology. India: Medical Book Company; 27th ed, 2008;95:440-456.
Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. The Lancet. 2012;380(9859):2095-2128. doi: 10.1016/S0140-6736(12)61728-0.
Brata Ghosh V, Jhamb U, Singhal R, Krishnan R. Common childhood poisonings and their outcome in a tertiary care center in Delhi. Indian J Pediatr. 2013;80(6):516-518. doi: 10.1007/s12098-012-0879-5.
Roy RN, Shrivastava P, Das DK, Saha I, Sarkar AP. Burden of hospitalized pediatric morbidity and utilization of beds in a tertiary care hospital of Kolkata, India. Indian J Comm Med. 2012;37(4):252. doi: 10.4103/0970-0218.103474.
Jayashree M, Singhi S. Changing trends and predictors of outcome in patients with acute poisoning admitted to the intensive care. J Trop Pediatr. 2011;57(5):340-346. doi: 10.1093/tropej/fmq099.
Kohli U, Kuttiat VS, Lodha R, Kabra SK. Profile of childhood poisoning at a tertiary care centre in North India. Indian J Pediatr. 2008;75(8):791. doi: 10.1007/s12098-008-0105-7.
Budnitz DS, Lovegrove MC. The last mile: taking the final steps in preventing pediatric pharmaceutical poisonings. J Pediatr. 2012;160(2):190-192. doi: 10.1016/j.jpeds.2011.09.020.
Suvedi BK. A retrospective study of poisoning cases at Bir Hospital, Nepal J Inst Med. 1990;12:296-302.
Lall SB. Accidental pediatric poisoning--a preventable medical emergency. Indian J Pediatr. 1998;65(3):363-364. doi: 10.1007/bf02761128.
Branche C, Ozanne-Smith J, Oyebite K, Hyder AA. World report on child injury prevention. World Health Organization; 2008;123-142.
Singh S, Singhi S, Sood NK, Kumar L, Walia BN. Changing pattern of childhood poisoning (1970-1989): experience of a large north Indian hospital. Indian Pediatr. 1995;32:331.
Dutta AK, Seth A, Goyal PK, Aggarwal V, Mittal SK, Sharma R, Bahl L, Thakur JS, Verma M, Chhatwal J, Chacko B. Poisoning in children: Indian scenario. Indian J Pediatr. 1998;65(3):365-370. doi: 10.1007/BF02761129.
Desalew M, Aklilu A, Amanuel A, Addisu M, Ethiopia T. Pattern of acute adult poisoning at Tikur Anbessa specialized teaching hospital, a retrospective study, Ethiopia. Human Experiment Toxicol. 2011;30(7):523-527. doi: 10.1177/0960327110377520.
Gupta SK, Peshin SS, Srivastava A, Kaleekal T. A study of childhood poisoning at national poisons information centre, All India Institute of Medical Sciences, New Delhi. J Occupational Health. 2003;45(3):191-196. doi: 10.1539/joh.45.191.
Balan B, Lingam L. Unintentional injuries among children in resource poor settings: where do the fingers point. Arch Dis Childhood. 2012;97(1):35-38. doi: 10.1136/archdischild-2011-300589.
Sharma A, Dishant VG, Kaushik JS, Mittal K. Aluminum phosphide (celphos) poisoning in children: A 5-year experience in a tertiary care hospital from northern India. Indian J Critical Care Med. 2014;18(1):33. doi: 10.4103/0972-5229.125434.
Singh SP, Aggarwal AD, Oberoi SS, Aggarwal KK, Thind AS, Bhullar DS, et al. Study of poisoning trends in north India–a perspective in relation to world statistics. J Forensic Legal Med. 2013;20(1):14-18. doi: 10.1016/j.jflm.2012.04.034.
Gupta S, Govil YC, Misra PK, Nath R, Srivastava KL. Trends in poisoning in children: experience at a large referral teaching hospital. Nat Med J India. 1998;11:166-168.
Sinno D, Majdalani M, Chatila R, Musharrafieh U, Al‐Tannir M. The pattern of self‐poisoning among Lebanese children and adolescents in two tertiary care centres in Lebanon. Acta Paediatrica. 2009;98(6):1044-1048. doi: 10.1111/j.1651-2227.2009.01251.x.
Franklin RL, Rodgers GB. Unintentional child poisonings treated in United States hospital emergency departments: national estimates of incident cases, population-based poisoning rates, and product involvement. Pediatr. 2008;122(6):1244-1251. doi: 10.1542/peds.2007-3551.
Rodgers GC, Matyunas NJ. Poisonings: Drugs, chemicals, and plants. Nelson Textbook of Pediatrics: Editors: Behrman RE, Kliegmen RM, Jenson HB. WB Saunders. Philadelphia. 2004:2362-2374.
Gupta SK, Peshin SS, Srivastava A, Kaleekal T. A study of childhood poisoning at national poisons information centre, All India Institute of Medical Sciences, New Delhi. J Occupational Health. 2003;45(3):191-196. doi: 10.1539/joh.45.191.
Gauvin F, Bailey B, Bratton SL. Hospitalizations for pediatric intoxication in Washington State, 1987-1997. Arch Pediatr Adol Med. 2001;155(10):1105-1110. doi: 10.1001/archpedi.155.10.1105.
Alazab RM, Elmougy MT, Fayad RA, Abdelsalam HF, Mohamed AS. Risk factors of acute poisoning among children: a study at a poisoning unit of a university hospital in Egypt. South East Asia J Public Health. 2012;2(2):41-47. doi: 10.3329/seajph.v2i2.15943.
Paudyal BP. Poisoning: pattern and profile of admitted cases in a hospital in central Nepal. JNMA J Nepal Med Assoc. 2005;44(159):92-96.
Gajalakshmi V, Peto R. Suicide rates in rural Tamil Nadu, South India: verbal autopsy of 39,000 deaths in 1997–98. Int J Epidemiol. 2007;36(1):203-207. doi: 10.1093/ije/dyl308.
Venkatesh C, Sriram P, Adhisivam B, Mahadevan S. Clinical profile of children with kerosene aspiration. Tropical Doc. 2011;41(3):179-180. doi: 10.1258/td.2011.110093.
WHO mortality database: tables. Geneva, World Health Organization. Available at https://apps.who.int/healthinfo/statistics/mortality/whodpms/params_ex.php. Accessed on July 20, 2020
Linnan M, Pham VC, Rahman F, Rahman A, Shafinaz S, Sitti-Amorn C, et al. Child mortality and injury in Asia: survey results and evidence. Innocenti Working Papers, No. 2007/06. doi: 10.18356/f28cffe5-en.
National Health Profile, 2019. Available at https://www.thehinducentre.com/resources/article29841374.ece/binary/8603321691572511495.pdf. Accessed on July 20 2020.
Du NT, Due B, Due P. Epidemiology of acute poisonings in Vietnam. J Toxicol Clin Toxicol. 2001; 39:527-528.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


