Cranial ultrasound in high-risk neonates and their neurodevelopmental outcome
Abstract
Introduction: With the advancement in neonatal care over the last two decades, neonatal mortality is decreased but simultaneously there is an increase in the adverse outcomes including neurodevelopmental abnormalities in the high-risk neonates.
Purpose: To evaluate the association between cranial ultrasound findings and the clinical neurodevelopmental outcome among high-risk neonates at 12 months (corrected gestational age in preterm infants) and to assess the various perinatal risk factors associated with neurodevelopmental outcome.
Material and Methods: 123 high-risk neonates admitted in NICU were enrolled. Cranial ultrasound was performed and morphology was noted. The neurodevelopmental assessment was done using DDST Test II at 12 months age and these neonates were labeled as normal or abnormal based on the findings. Association between the two non-parametric variables was seen using the Pearson Chi-square test.
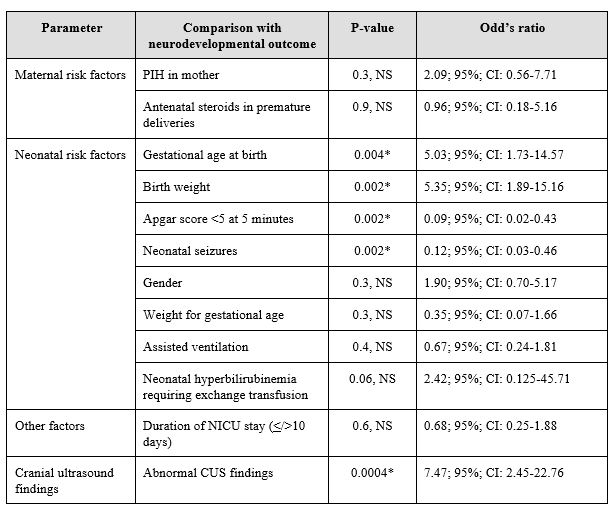
Results: There was a statistically significant association between clinical neurodevelopmental outcome and gestational age at birth; birth weight; Apgar score <5 at 5 minutes; neonatal seizures; and abnormal cranial ultrasound findings (p<0.05), while the association with all other studied parameters were found to be statistically not significant (p>0.05). The sensitivity of CUS was 89.2%, specificity 47.3%, positive predictive value 89.2%, and negative predictive value 47.3%.
Conclusions: The neurodevelopmental outcome in high-risk neonates was associated with gestational age at birth; birth weight; Apgar score at 5 minutes; neonatal seizures and abnormal cranial ultrasound findings. The current study recommend the use of cranial ultrasound for the prediction of neurodevelopmental abnormalities especially in neonates with above risk factors.
Downloads
References
Public Health Foundation of India, All India Institute of Medical Sciences, Save the Children. Zodpey S, Paul VK, editors. State of India’s Newborns (SOIN) 2014 – A Report. New Delhi: PHFI, AIIMS, SC; 2014.
Beaino G, Khoshnood B, Kaminski M, Pierrat V, Marret S, Matis J, et al; EPIPAGE Study Group. Predictors of cerebral palsy in very preterm infants: the EPIPAGE prospective population-based cohort study. Dev Med Child Neurol. 2010;52(6):e119-e125. doi: 10.1111/j.1469-8749.2010.03612.x.
Backes CH, Markham K, Moorehead P, Cordero L, Nankervis CA, Giannone PJ. Maternal preeclampsia and neonatal outcomes. J Pregnancy. 2011;2011:214365. doi: 10.1155/2011/214365.
Spinillo A, Iasci A, Capuzzo E, Egbe TO, Colonna L, Fazzi E. Two-year infant neurodevelopmental outcome after expectant management and indicated preterm delivery in hypertensive pregnancies. Acta Obstet Gynecol Scand. 1994;73(8):625-629. doi: 10.3109/00016349409013455.
Sotiriadis A, Tsiami A, Papatheodorou S, Baschat AA, Sarafidis K, Makrydimas G. Neurodevelopmental Outcome After a Single Course of Antenatal Steroids in Children Born Preterm: A Systematic Review and Meta-analysis. Obstet Gynecol. 2015;125(6):1385-1396. doi: 10.1097/AOG.0000000000000748.
Carlo WA, McDonald SA, Fanaroff AA, Vohr BR, Stoll BJ, Ehrenkranz RA, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Association of antenatal corticosteroids with mortality and neurodevelopmental outcomes among infants born at 22 to 25 weeks' gestation. JAMA. 2011;306(21):2348-2358. doi: 10.1001/jama.2011.1752.
Ancel PY, Livinec F, Larroque B, Marret S, Arnaud C, Pierrat V, et al. Cerebral palsy among very preterm children in relation to gestational age and neonatal ultrasound abnormalities: the EPIPAGE cohort study. Pediatr. 2006;117(3):828-835. doi: 10.1542/peds.2005-0091.
Romeo DM, Brogna C, Sini F, Romeo MG, Cota F, Ricci D. Early psychomotor development of low-risk preterm infants: Influence of gestational age and gender. Eur J Paediatr Neurol. 2016;20(4):518-523. doi: 10.1016/j.ejpn.2016.04.011.
Hintz SR, Kendrick DE, Wilson-Costello DE, Das A, Bell EF, Vohr BR, et al; NICHD Neonatal Research Network. Early-childhood neurodevelopmental outcomes are not improving for infants born at <25 weeks' gestational age. Pediatr. 2011;127(1):62-70. doi: 10.1542/peds.2010-1150.
Boulet SL, Schieve LA, Boyle CA. Birth weight and health and developmental outcomes in US children, 1997-2005. Matern Child Health J. 2011;15(7):836-844. doi: 10.1007/s10995-009-0538-2.
van Os J, Wichers M, Danckaerts M, Van Gestel S, Derom C, Vlietinck R. A prospective twin study of birth weight discordance and child problem behavior. Biol Psychiatry. 2001;50(8):593-599. doi: 10.1016/s0006-3223(01)01085-x.
Bickle Graz M, Tolsa JF, Fischer Fumeaux CJ. Being Small for Gestational Age: Does it Matter for the Neurodevelopment of Premature Infants? A Cohort Study. PLoS One. 2015;10(5):e0125769. doi: 10.1371/journal.pone.0125769.
Goldenberg RL, Hoffman HJ, Cliver SP. Neurodevelopmental outcome of small-for-gestational-age infants. Eur J Clin Nutr. 1998;52(1):S54-S58.
Misra PK, Srivastava N, Malik GK, Kapoor RK, Srivastava KL, Rastogi S. Outcome in relation to Apgar score in term neonates. Indian Pediatr. 1994;31(10):1215-1218.
Finer NN, Robertson CM, Richards RT, Pinnell LE, Peters KL. Hypoxic-ischemic encephalopathy in term neonates: perinatal factors and outcome. J Pediatr. 1981;98(1):112-117. doi: 10.1016/S0022-3476(81)80555-0.
Tekgul H, Gauvreau K, Soul J, Murphy L, Robertson R, Stewart J, et al. The current etiologic profile and neurodevelopmental outcome of seizures in term newborn infants. Pediatr. 2006;117(4):1270-1280. doi: 10.1542/peds.2005-1178.
Pisani F, Leali L, Parmigiani S, Squarcia A, Tanzi S, Volante E, et al. Neonatal seizures in preterm infants: clinical outcome and relationship with subsequent epilepsy. J Matern Fetal Neonatal Med. 2004;16(2):51-53. doi: 10.1080/14767050410001727215.
Duan Y, Sun FQ, Li YQ, Que SS, Yang SY, Xu WJ, et al. Prognosis of psychomotor and mental development in premature infants by early cranial ultrasound. Ital J Pediatr. 2015;41:30. doi: 10.1186/s13052-015-0135-5.
O'Shea TM, Kuban KC, Allred EN, Paneth N, Pagano M, Dammann O, et al. Extremely Low Gestational Age Newborns Study Investigators. Neonatal cranial ultrasound lesions and developmental delays at 2 years of age among extremely low gestational age children. Pediatr. 2008;122(3):e662-e669. doi: 10.1542/peds.2008-0594.
Pinto-Martin JA, Riolo S, Cnaan A, Holzman C, Susser MW, Paneth N. Cranial ultrasound prediction of disabling and nondisabling cerebral palsy at age two in a low birth weight population. Pediatr. 1995;95(2):249-254. Erratum in: Pediatr. 2001;108(2):238.
Seme-Ciglenecki P. Predictive values of cranial ultrasound and assessment of general movements for neurological development of preterm infants in the Maribor region of Slovenia. Wien Klin Wochenschr. 2007;119(15-16):490-496. doi: 10.1007/s00508-007-0839-7.
Ng PC, Dear PR. The predictive value of a normal ultrasound scan in the preterm baby – A meta-analysis. Acta Paediatrica Scandinavica. 1990;79(3):286-291. doi: 10.1111/j.1651-2227.1990.tb11458.x.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


