Association between Serum Magnesium level and outcome in birth asphyxia
Abstract
Introduction: Magnesium (Mg) has been found to block the NMDA ion channel under resting conditions, occupying a binding site within the ion channel. The block is voltage-dependent and is overcome during axonal depolarization that occurs with hypoxia-ischemia. The systemic administration of magnesium after a stimulated hypoxic ischemia insult has been shown to limit neuronal injury in several animal models.
Material and Methods: Cross-sectional study conducted at the Nehru Hospital, BRD Medical College, Gorakhpur (UP) in the Neonatal Intensive Care Unit of the pediatric department.
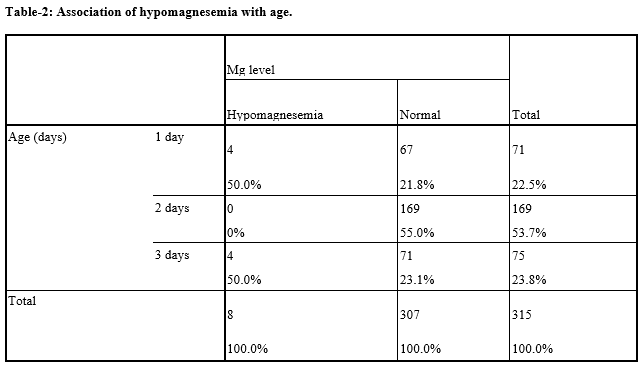
Result: The prevalence of hypomagnesemia was 2.5%. Hypomagnesemia was more on day 1 and day 3. Severe birth asphyxia had more prevalence of Hypomagnesaemia. On day one 4 out of 71 patients had hypomagnesemia. On day 2 no patient had hypomagnesemia, while on day three 4 patients had hypomagnesemia out of 75. A significant difference was found in hypomagnesemia on day 1 and day 2 as well as day 2 and day 3. No patient had an antenatal high-risk factor in mother who had hypomagnesemia; there was no significant association between high-risk factors and hypomagnesemia.
Conclusion: There should be more studies regarding hypomagnesemia in birth asphyxia and the association of hypomagnesemia with other parameters.
Downloads
References
Kumar A, Gupta A. Clinico-etiological and EEG profile of neonatal seizures. Indian J Pediatr. 2007;74(1):33-37. doi: 10.1007/s12098-007-0023-0.
Kumar A, Gupta V, Kacchawaha JS, Singla PN. Biochemical abnormalities in neonatal seizures. Indian Pediatr. 1995;32:424-428.
Antonucci R, Prcella A, and Pilloni MD. Perinatal asphyxia in term newborn. J Pediatr Neonat Individual Med. 2014;3(2):e030269. doi: 10.7363/030269.
Aslam HM, Saleem S, Afzal R, Iqbal U, Saleem SM, Shaikh MW, et al. Risk factors of birth asphyxia. Ital J Pediatr. 2014;40(1):94. doi: 10.1186/s13052-014-0094-2.
Manual of neonatal care. Cloherty 7th edition. Incidence rate of neonatal seizure. 2012 by Lippincott Williams & Wilkins, a Wolters Kluwer.
Jajoo D, Kumar A, Shankar R, Bhargana. Effect of birth asphyxia in serum Magnesium levels in neonate. Indian J Pediatr. 1995;62(4):455-459. doi: 10.1007/BF02755067.
Tekgul H, Gauvreau K, Soul J, Murphy L, Robertson R, Stewart J, et al. The current etiologic profile and neurodevelopmental outcome of seizures in term newborn infants. Pediatr. 2006;117(4):1270-1280. doi: 10.1542/peds.2005-1178.
Choi DW, Rothman SM. The role of glutamate neurotoxicity in hypoxic-ischemic neuronal death. Ann Rev Neurosci. 1990;13(1):171-182. doi: 10.1146/annurev.ne.13.030190.001131.
Ichiba H, Yokoi T, Tamai H, Ueda T, Kim TJ, Yamano T. Neurodevelopment outcome of infants with birth asphyxia treated with magnesium sulfate. Pediatr. 2006;48(1):70-75. doi: 10.1111/j.1442.2006.02167.x.
Gulogfnard JP, Sulyok E. Renal Morphogenesis and development of renal function. In: gleason CA, Devaskar SU, eds. Avery’s Disease of the Newborn. 9th ed. Philadelphia, PA; Elsevier Saunders; 2012: 1165-1175.
Douglas-Escobar MN, Weiss MD. Hypoxic-ischemic encephalopathy: A review for the clinician. JAMA Pediatr. 2015;169(4):397-403. doi: 10.1001/ jamapediatrics.2014.32659.
Reinhart RA. Magnesium metabolism. A review with special reference to the relationship between intracellular content and serum levels. Arch Int Med. 1988;148(11):2415-2420. doi: 10.1001/archinte.148.11.2415.
Musso CG. Magnesium metabolism in health and disease. Int Urol Nephrol. 2009;41(2):357-362. doi: 10.1007/s11255-009-9548-7.
Kaze FF, Stoermann CC. Magnesium metabolism disturbances Rev Med Suisse. 2007;3(101):605-6, 608, 610-1.
Moe SM. Disorders involving calcium, phosphorus and magnesium. Prim Car. 2008;35(2):215-237. doi: 10.1016/j.pop.2008.01.007.
Rouse DJ, Hirtz DG, Thom E, Varner MW, Spong CY, Mercer BM. et al. A randomized, controlled trial of magnesium sulfate for the prevention of cerebral palsy. N Engl J Med. 2008;359(9):895-905. doi: 10.1056/NEJMoao8201187.
Doyle LW, Crowther CA, Middleton P, Marret S, Rouse D. Magnesium sulphate for woman at risk of preterm birth for neuroprotection of the fetus. Cochrane Database Syst rev. 2009; 21 (1): CD004661.doi:10.1002/14651858.CD004661.
Tsang RC, Oh W. Serum magnesium levels in low birth weight infants. Am J Dis Child. 1970;120(1):44-48. doi:10.1001/archpedi.1970.02100060078010.
Maged M, Costantine MD. Effects of antenatal exposure to magnesium sulphate on neuroprotection and mortality in preterm infants. Meta-analysis. Obstet Gynecol. 2009;114(2):354-364. doi: 10.1097/AOG.obo13e3181ae98c2.
Demirci J, Schmella M, Glasser M, Bodnar L, Himes KP. Delayed Lactogenesis II and potential utility of antenatal milk expression in women developing late-onset preeclampsia: a case series. BMC Pregnancy Childbirth. 2018;18(1):68. doi: 10.1186/s12884-018-1693-5.
Stevenson TJ, Trinh T, Kogelschatz C, Fujimoto E, Lush ME, Piotrowski T, et al. Hypoxia disruption of vertebrate CNS pathfinding through ephrinB2 Is rescued by magnesium. PLoS Genet. 2012;8(4):e1002638. doi: 10.1371/journal.pgen.1002638.
Abbassi-Ghanavati M, Alexander JM, McIntire DD, Savani RC, Leveno KJ. Neonatal effects of magnesium sulfate given to the mother. Am J Perinatol. 2012;29(10):795-800. doi: 10.1055/s-0032-1316440.
Gathwala G, Khera A, Singh I. Magnesium therapy in birth asphyxia. Indian J Pediatr. 2006;73(3):209-212. doi: 10.1007/BF02825482.
Bhat MA, Charoo BA, Bhat JI, Ahmad SM, Ali SW. Magnesium sulfate in severe perinatal asphyxia: a randomized, placebo-controlled trial. Pediatr. 2009;123(5):e764-e769.
Galvin KA, Oorschot DE. Continuous low-dose treatment with brain-derived neurotrophic factor or neurotrophin-3 protects striatal medium spiny neurons from mild neonatal hypoxia/ischemia: a stereological study. Neurosci. 2003;118(4):1023-1032. doi: 10.1016/s0306-4522(03)00066-6.
Kumr D, Yelamali B, Pol Y. Serum calcium and magnesium levels in predicting short term outcome of term neonates with hypoxic ischemic encephalopathy. Med Innovatica. 2018;7(1):44-47.
Elizabeth KE, Krishnan V, Zachariah P. Auxologic, Biochemical and Clinical (ABC) Profile of Low Birth Weight Babies—A 2-year Prospective Study. J Trop Pediatr. 2007;53(6):374-382.
Saggesc G, Baroncelli GI, Bertelloni S, Cipolloni C. Intact parathyroid hormone levels during pregnancy, in healthy term neonates and in hypocalcemic preterm infants. Acta Paediatr Scan. 1991;80(1):36-41. doi: 10.1111/j.1651-2227.1991.tb11726.x.
Rubin LP, Posillico JT, Anast CS, Brown EM. Circulating levels of biologically active and immunoreactive intact parathyroid hormone in human newborns. Pediatr Res 1991;29(2):201-207. doi: 10.1203/00006450-199102000-00020.
Mimouni F, Loughead JL, Tsang RC, Khoury J, et al. Postnatal surge in serum calcitonin concentrations: no contribution to neonatal hypocalcaemia in infants of diabetic mothers. Pediatr Res 1990;28(5):493-495. doi: 10.1203/00006450-199011000-00015.
Ilves P, Blennow M, Kütt E, Mägi ML, Kudrjavtseva G, Lagercrantz H, Talvik T. Concentrations of magnesium and ionized calcium in umbilical cord blood in distressed term newborn infants with hypoxic‐ischemic encephalopathy. Acta Pædiatrica. 1996;85(11):1348-1350. doi: 10.1111/j.1651-2227.1996.tb13923.x.
Yadav N, Damke S. Study of risk factors in children with birth asphyxia. Int J Contemp Pediatr. 2017;4(2):518-526. doi: 10.18203/2349-3291.ijcp20170701.
Dalal CA, Bodar NL. A study on birth asphyxia at tertiary health centre. Natl J Med Res. 2013;3(4):374-376.
Padaychee N, Ballot DE. Outcomes of neonates with perinatal asphyxia at a tertiary academic hospital in Johannesburg. South Africa. South African J Ch Health. 2013;7(3):89-94.
Shalev H, Phillip M, Galil A, Carmi R, Landau D. Clinical presentation and outcome in primary familial hypomagnesaema. Arch Dis Child. 1998;78(2):127-130. doi: 10.1136/adc.78.2.127.
Mathias RS, Nguajen HT, Zhang MY, Portale AA. Reduced expression of the renal calcium-sensing receptor in rats with experimental chronic renal insufficiency. J Am Soc Nephrol. 1998;9(11):2067-2074.
Suganthi V, Vikneshwari K, Thivya G. Prevalence of hypomagnesemia in neonatal seizures in a tertiary care hospital in South India. Pediatr Rev: Int J Pediatrics Res. 2017;4(01):64-68. doi:10.17511/ijpr.2017.01.13.
Saha D, Ali MA, Haque MA, Ahmed MS, Sutradhar PK, Latif T, Sarkar D, Husain F. Association of hypoglycemia, hypocalcemia and hypomagnesemia in neonates with perinatal asphyxia. Mymensingh Med J. 2015;24(2):244-250.
Khalesi N, Namiranian P, Farahani Z. The Frequency of Early and Late Hypocalcemia Among Hospitalized Newborns in An Iranian Hospital. Shiraz E Med J. 2015;16(6). doi: 10.17795/semj28080.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


