Nasal intermittent positive pressure ventilation in neonates with meconium aspiration syndrome
Abstract
Background: Nasal intermittent positive pressure ventilation ( NIPPV) as primary respiratory support in neonates with meconium aspiration syndrome (MAS) has not been studied. The present study applied the use of NIPPV as a treatment modality in MAS and tried to identify factors predicting NIPPV failure.
Objective: The aim was to identify failure rates of MAS on NIPPV and potential predictors of NIPPV failure.
Design: Observational analytical study.
Methods: 86 neonates were admitted during the study period of 2 years of which 60 were included and NIPPV was applied as the primary modality of respiratory support with available ventilators. Outcome variables were compared between the MAS infants who failed NIPPV and those who were successfully managed with NIPPV.
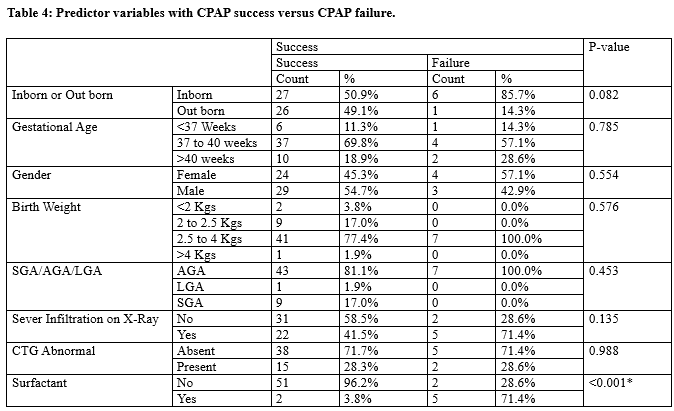
Results: 7 neonates (11.7%) out of 60 enrolled neonates failed on NIPPV. There was a significant decrease in Downe score, respiratory rate, heart rate, fio2 requirement after 6 hours compared to a baseline measurement (p<0.01). On univariate analysis factors associated with NIPPV failure were high Fio2, high PEEP, at one hour of starting NIPPV (p<0.05). However, on logistic regression none of the factors were predicting failure independently.
Conclusion: NIPPV applied early may reduce the need for mechanical ventilation in neonates with moderate to severe MAS.
Downloads
References
Dargaville PA. Respiratory support in meconium aspiration syndrome. Int J of Paediatrics. 2012:2012:965159. doi: 10.1155/2012/965159.
Singh BS, Clark RH, Powers RJ, Spitzer AR. Meconium aspiration syndrome remains a significant problem in the NICU: outcomes and treatment patterns in term neonates admitted for intensive care during a ten-year period. J Perinatol. 2009;29(7):497-503. doi: 10.1038/jp.2008.241.
Wiswell TE, Bent RC. Meconium staining and the meconium aspiration syndrome: unresolved issues. Pediatr Clin North Am. 1993;40(5):955-981. doi: 10.1016/s0031-3955(16)38618-7.
Dargaville PA, Copnell B. The epidemiology of meconium aspiration syndrome: incidence, risk factors, therapies, and outcome. Pediatr. 2006;117(5):1712-1721. doi: 10.1542/peds.2005-2215.
Goldsmith JP. Continuous positive airway pressure and conventional mechanical ventilation in the treatment of meconium aspiration syndrome. J Perinatol. 2008;28(3):S49-55. doi: 10.1038/jp.2008.156.
Lakshminrusimha S, Russell JA, Steinhorn RH, Ryan RM, Gugino SF, Morin FC, et al. Pulmonary arterial contractility in neonatal lambs increases with 100% oxygen resuscitation. Pediatr Res. 2006;59(1):137-141. doi: 10.1203/01.pdr.0000191136.69142.8c.
SAUGSTAD OD. Oxygen toxicity in the neonatal period. Acta Paediatrica. 1990;79(10):881-892. doi: 10.1111/j.1651-2227.1990.tb11348.x.
Bhagwat P, Murki S, Mehta A, Oleti T, Gannavaram D. Continuous positive airway pressure in meconium aspiration syndrome: an observational study. J Clin Neonatol. 2015;4(2):96-100. doi: 10.4103/2249-4847.154107.
Ower LS, Morley B J. Nasal intermittent positive pressure ventilation in preterm infants :equipment, evidence and sychronization. Semin fetal neonatal Med. 2016,21(3):146-153. doi: 10.1016/j.siny.2016.01.003.
Ower LS, Morley CJ, Dawson JA ,Davis PG, Effects of non synchronised nasal intemittent positive pressure ventilation on spontaneous breathing in preterm infants. Arch Dis child Fetal Neonatal Ed. 2011;96(6):F422-F428.
Kugelman A, Feferkorn I, Riskin A, Chistyakov I, Kaufman B, Bader D. Nasal intermittent mandatory ventilation versus nasal continuous positive airway pressure for respiratory distress syndrome: a randomized, controlled, prospective study. J Pediatr. 2007;150(5):521-526.
Sai Sunil Kishore M, Dutta S, Kumar P. Early nasal intermittent positive pressure ventilation versus continuous positive airway pressure for respiratory distress syndrome. Acta Paediatrica. 2009;98(9):1412-1415. doi: 10.1111/j.1651-2227.2009.01348.x.
Meneses J, Bhandari V, Alves JG, Herrmann D. Noninvasive ventilation for respiratory distress syndrome: a randomized controlled trial. Pediatr. 2011;127(2):300-307. doi: 10.1542/peds.2010-0922.
Ramanathan R, Sekar KC, Rasmussen M, Bhatia J, Soll RF. Nasal intermittent positive pressure ventilation after surfactant treatment for respiratory distress syndrome in preterm infants< 30 weeks’ gestation: a randomized, controlled trial. J Perinatol. 2012;32(5):336-343. doi: 10.1038/jp.2012.1.
Lampland AL, Meyers PA, Worwa CT, Swanson EC, Mammel MC. Gas exchange and lung inflammation using nasal intermittent positive-pressure ventilation versus synchronized intermittent mandatory ventilation in piglets with saline lavage-induced lung injury: an observational study. Crit Care Med. 2008;36(1):183-187. doi: 10.1097/01.CCM.0000295311.61378.7D.
Pandita A, Murki S, Oleti TP, Tandur B, Kiran S, Narkhede S, Prajapati A. Effect of nasal continuous positive airway pressure on infants with meconium aspiration syndrome: a randomized clinical trial. JAMA Pediatr. 2018;172(2):161-165. doi: 10.1001/jamapediatrics.2017.3873.
Davis PG, Lemyre ,Kirpalani H ,Nasal intermittent positive pressure ventilation (NIPPV)versus nasal continuous positive airway pressure (NCPAP)for preterm neonates after extubation.Cochrane database syst Rev,2011:(3)CD003212. doi: 10.1002/14651858.CD003212.pub3.
El-Sayed SA, Shehab MM, Ahmady MM, Baraka A. Early Management of Newborn with Meconium Aspiration Syndrome Using Continuous Positive Airway Pressure as a Special Modality. Int J Pharm Phytopharm Res. 2018;8(1):16-20.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


