Screening for fecal occult blood loss in severely malnourished children
Abstract
Introduction: PEM is the most important and basic hurdle in the triple-M complex of malnutrition, morbidity, and mortality. Very high mortality has been reported in severe PEM. PEM is found to account for about 4 million deaths in children. The study aimed to perform a fecal occult blood test in patients in the age group of six months to five years and also to identify the conditions associated with fecal occult blood loss in pem patients.
Materials and Methods: A total of 100 indoor patients of PEM admitted in our pediatric ward were taken as subjects in this study. According to WHO and IAP classification of PEM, severe malnutrition (marasmus, kwashiorkor, and marasmic kwashiorkor) were taken as study group; and mild grades of PEM (grade I and grade II) were taken as a control group.
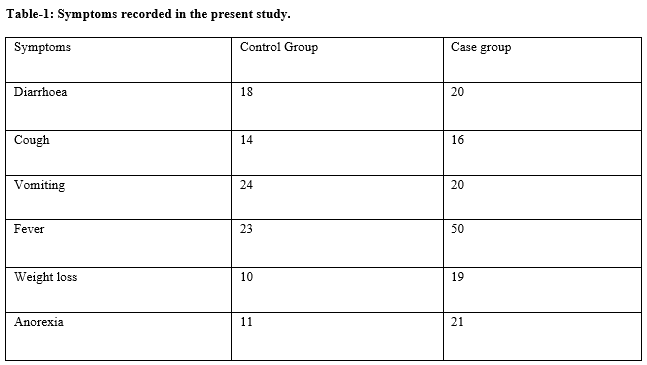
Results: In severe PEM, marasmus (83%) was more common followed by kwashiorkor (14%) and marasmic kwashiorkor (3%); however in mild grades of PEM, grade I PEM was found in 58% and grade II PEM was found in 42%. In severe PEM, pallor (64%), hair changes (38%), and tachypnoea(31%) were major clinical signs; while tachypnoea(36%), dehydration (26%), and pallor (20%} were major clinical signs in patients with mild grades of PEM.
Conclusion: A positive fecal occult blood test (FOBT) is strongly associated with moderate to severe anemia in severe PEM patients. So all patients having a positive FOBT should have a hemogram profile done and then appropriately treated for anemia.
Downloads
References
Bhutia DT. Protein energy malnutrition in India: the plight of our under five children. J Family Med Prim Care. 2014;3(1):63-67. doi: 10.4103/2249-4863.130279.
Phengxay M, Ali M, Yagyu F, Soulivanh P, Kuroiwa C, Ushijima H. Risk factors for protein–energy malnutrition in children under 5 years: study from Luangprabang province, Laos. Pediatr Int. 2007;49(2):260-265. doi: 10.1111/j.1442-200X.2007.02354.x.
Purohit L, Sahu P, Godale LB. Nutritional status of under-five children in a city of Maharashtra: a community based study. Int J Community Med Public Health. 2017,4(4):1171-1178. doi: 10.18203/2394-6040.ijcmph20171344.
Snehalatha P. Study to assess the knowledge of mothers of under five children regarding protein-energy malnutrition in selected area of Raichur with a view to develop health educatioon module. RGUHS, 2005.
Stoltzfus RJ. Defining iron-deficiency anemia in public health terms: a time for reflection. J Nutr. 2001;131(2):565S-7S. doi: 10.1093/jn/131.2.697S.
Kumar GB. The study of severe anaemia with respect to etiology clinical features and hematological changes in infancy and childhood at vims hospital. 2011.
Bhutta ZA, Berkley JA, Bandsma RH, Kerac M, Trehan I, Briend A. Severe childhood malnutrition. Nat Rev Dis Prim. 2017;3:1-18. doi: 10.1038/nrdp.2017.67.
Jain S, Das S, Gupta P. Fecal occult blood screening in children with severe malnutrition. Indian Pediatr. 2007;44:913-915.
Bhatia V, Puri S, Swami H, Gupta M, Singh G. Malnutrition among under six children in Chandigarh: scarcity in plenty. J Clin Diagnos Res. 2007;1(6):483-487.
Hamidu J, Salami H, Ekanem A, Hamman L. Prevalence of protein-energy malnutrition in Maiduguri, Nigeria. Af J Biomed Res. 2003;6(3). doi: 10.4314/ajbr.v6i3.54039.
Copyright (c) 2021 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


