Thyroid profile in patients of thalassemia with multiple blood transfusions and high serum ferritin: a cross-sectional study
Abstract
Introduction: Beta-thalassemia major patients undergo regular blood transfusion resulting in growth faltering and various endocrine problems including thyroid dysfunction due to iron overload in the body. This study was conducted to determine the frequency of thyroid dysfunction in children presenting with Beta-thalassemia major on regular blood transfusions.
Materials and methods: Sixty children were included with proven beta-thalassemia major who reported to the Department of Pediatrics, VIMS, and RC, Bangalore. Inclusion criteria: 1.Children 4 to 18 years age group .2.The child received transfusions for more than 2 years. 3.Children with serum ferritin level >700.
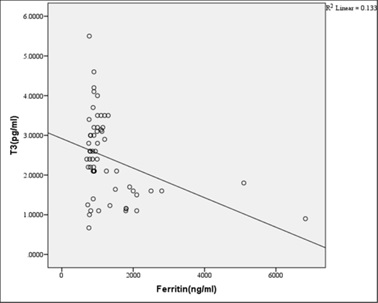
Results: In this study, four patients(6.8%) had overt hypothyroidism, eight patients(13.6%) had subclinical hypothyroidism and 47 patients(79.7%) had euthyroid status. There was a positive correlation between Ferritin and T4, TSH levels. i.e., with an increase in Ferritin level, there was an increase in T4, TSH levels, and vice versa. However, the correlation was significant with TSH. There was a significant negative correlation between Ferritin and T3 levels. i.e with an increase in Ferritin level, there was a decrease in T3 levels and vice versa.
Conclusion: Thyroid dysfunction can exist in thalassemia patients on multiple transfusions and chelation therapy with high serum ferritin levels. Detection of hypothyroidism is important as inexpensive oral replacement therapy is readily available. Hence regular screening of beta-thalassemia major patients for Serum T3, Serum T4, Serum TSH for early detection and timely treatment could improve the life expectancy and quality of life of these patients.
Downloads
References
Patricia J. Giardina SR. Thalassemia Syndromes. Hoffman: Hematology: Basic Principles And Practice. 6th ed. Philadelphia: Elsevier Saunders; c2013.
Vichinsky EP. Changing patterns of thalassemia worldwide. Ann N Y Acad Sci. 2005;1054(1):18-24. doi: 10.1196/annals.1345.003.
Madan N, Sharma S, Sood SK, Colah R, Bhatia LH. Frequency of β-thalassemia trait and other hemoglobinopathies in northern and western India. Indian J Hum Genet. 2010;16(1):16-25. doi:10.4103/0971-6866.64941.
Balgir RS. Genetic epidemiology of the three predominant abnormal hemoglobins in India. J Assoc Physicians India. 1996;44(1):25-28.
Saka N, Sükür M, Bundak R, Anak S, Neyzi O, Gedikoğlu G. Growth and puberty in thalassemia major. J Pediatr Endocrinol Metab. 1995;8(3):181-186. doi: 10.1515/jpem.1995.8.3.181.
Modell B, Letsky EA, Flynn DM, Peto R, Weatherall DJ. Survival and desferrioxamine in thalassaemia major. Br Med J (Clin Res Ed). 1982;284(6322):1081-1084. doi: 10.1136/bmj.284.6322.1081.
Cappellini MD, Cohen A, Eleftheriou A, Piga A, Porter J, Taher A. Guidelines for the Clinical Management of Thalassaemia [Internet]. 2nd Revised ed. Nicosia (CY): Thalassaemia International Federation; 2008.
Galanello R, Origa R. Beta-thalassemia. Orphanet J Rare Dis. 2010;5(1):11. doi: 10.1186/1750-1172-5-11.
Tiosano D, Hochberg Z. Endocrine Complications of Thalassaemia. J Endocrinol Invest.2001;24(9):716-723. doi:10.1007/BF03343916.
Karamifar H, Shahriari M, Amirhakimi GH. Failure of Puberty and Linear Growth in Beta Thalassemia Major. Turkish J Hematol. 2005;22(2):65-69.
Roth C, Pekrun A, Bartz M, Jarry H, Eber S, Lakomek M, Schröter W. Short stature and failure of pubertal development in thalassaemia major: evidence for hypothalamic neurosecretory dysfunction of growth hormone secretion and defective pituitary gonadotropin secretion. Eur J Pediatr. 1997;156(10):777-783. doi: 10.1007/s004310050711.
Soliman AT, elZalabany M, Amer M, Ansari BM. Growth and pubertal development in transfusion-dependent children and adolescents with thalassaemia major and sickle cell disease: a comparative study. J Trop Pediatr. 1999;45(1):23-30. doi: 10.1093/tropej/45.1.23.
Landau H, Matoth I, Landau-Cordova Z, Goldfarb A, Rachmilewitz EA, Glaser B. Cross-sectional and longitudinal study of the pituitary-thyroid axis in patients with thalassaemia major. Clin Endocrinol (Oxf). 1993;38(1):55-61. doi: 10.1111/j.1365-2265.1993.tb00973.x.
S. Mariotti, F. Pigliaru, M. C. Cocco, A. Spiga, S. Vaquer and M. E. Lai. β-Thalassemia and Thyroid Failure: Is There a Role for Thyroid Autoimmunity?. Pediatr Endocrinol Rev. 2011;8(2):307-309.
De VS, Vullo C, Urso L, Rigolin F, Cavallini A, Caramelli K, et al. Clinical Experience Using the Androderm Testosterone Transdermal System in Hypogonadal Adolescents and Young Men with Beta Thalassemia Major. J Pediatr Endocrinol Metabol.1998;11(3):891-900.
Agarwal MB, Shah S, Vishwanathan C, Rajadhyaksha G, Bhave AA, Dube SR et al. Thyroid dysfunction in multi-transfused iron loaded thalassemia patients. Indian Pediatr. 1992;29(8):997-102.
Jain M, Sinha RS, Chellani H, Anand NK. Assessment of thyroid functions and its role in body growth in thalassemia major. Indian Pediatr. 1995;32(2):213-219.
De Sanctis V, Tanas R, Gamberini MR, Sprocati M, Govoni MR, Marsella M. Exaggerated TSH response to TRH ("sub-biochemical" hypothyroidism) in prepubertal and adolescent thalassaemic patients with iron overload: prevalence and 20-year natural history. Pediatr Endocrinol Rev. 2008;6(1):170-173.
V. De Sanctis, M. Ughi, A. Pinamonti, M. Zachmann, T. Torresani, R. Gamberini, et al. “Growth Retardation in Thalassemia Major,” In: A. Prader and R. Rappaport, Eds., Clinical Issues in Growth Disorders: Evaluation, Diagnosis and Therapy, Freund publishing House Ltd, London, 1994, pp 31-47.
Jaipuria R,Nigam RK, Malik R, Shrivastava A, Balani S, Tripathi A. Assessment of thyroid function in children with beta-thalassemia major and its correlation with serum ferritin and transfusion index. J Evol of Med and Dental Sci. 2014;3(4):847-854. doi: 10.14260/jemds/2014/1914.
D Parijat, Mistry R, Wright C, Pancham S, Burbridge W, Gangopadhayay K et al. A Review of Endocrine Disorders in Thalassaemia. OJEMD. 2014;4(2):25-34. doi:10.4236/ojemd.2014.42003.
Eshragi P, Tamaddoni A, Zarifi K, Mohammadhasani A, Ahminzadeh M. Thyroid function in major thalassemia patients: is it related to height and chelation therapy. Capsian J Intern Med. 2011;2(1):189-193.
V. Chirico, A. Lacquaniti, V. Salpietro, N. Luca, V. Ferraù, B. Piraino et al. Thyroid Dysfunction in Thalassemic Patients: Ferritin as Prognostic Marker and Combined Iron Chelators as Ideal Therapy. Europe J Endocrinol. 2013; 169(6):785-793. doi: 10.1530/eje-13-0627.
Solanki US, Bhargava AK, Adole PS. Assessment of thyroid dysfunction in multi-transfused children of beta thalassemia major with iron overload. World J Pharmacy Pharmaceutical Sci. 2013; 3(8): 2177-2183.
Kundu D, Ray D, Ghosh S, Chowdhury DG, Dutta S, Dhar A. Relation of elevated serum ferritin levels to hypothyroidism in children with beta-thalassemia major. Int J Med Res Rev. 2016;4(12):2120-2124. doi:10.17511 /ijmrr.2016.i12.07.
Copyright (c) 2021 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


