The pattern of admission and their related outcomes in NICU of a tertiary care teaching hospital, Udaipur, Rajasthan, India
Abstract
Introduction: To achieve MDG4 (Millennium Developmental Goals-4), a substantial reduction in early neonatal deaths will be required. The first steps in improving early neonatal survival are to document the number and rate of deaths and identify their common causes. As per the National Family Health Survey-3 report, the current neonatal mortality rate (NMR) in India is 39 per 1000 live births, neonatal deaths account for nearly 77% of all infant deaths (57/1000) and nearly half of under-five child deaths (74/1000). This study was undertaken to study the disease pattern and outcome of neonates admitted to the neonatal intensive care unit (NICU) of a tertiary care teaching hospital located in Udaipur, Rajasthan.
Material and methods: The age, sex, gestational age, and morbidity and mortality profile of all NICU admissions in 5 years was determined and the difference between Inborn (those born in the Teaching Hospital) and Out born was calculated. Morbidity risk factors to reduce NMR in Udaipur were determined.
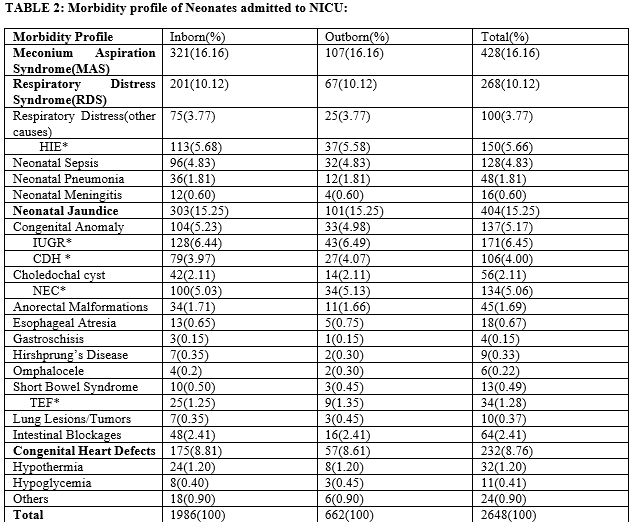
Results: A total of 2648 neonates were admitted to NICU during the study period, out of which none were excluded from the study. The ratio of Male to Female admitted was 1.30:1. The major causes of morbidity were Meconium Aspiration Syndrome (16.16%), Respiratory Distress Syndrome(10.12%), Cong. Heart Defects(8.76%), Neonatal Sepsis(4.83%) and Hypoxic-Ischemic Encephalopathy(5.66%). In this study, the overall mortality rate was 9.96%. Most of the Deaths were due to MAS(25.75%), RDS(15.90%), Neonatal Sepsis(10.22%), and HIE(12.87%). Neonates with birth weight <1000g had poor outcomes compared to neonates with birth weight >2500g.
Conclusion: This study identified Prematurity, Extremely low birth weight, MAS, and Neonatal Sepsis as major causes of Morbidity and MAS, RDS as the major contributors to neonatal mortality. Improving antenatal care, maternal health, and timely referral of high-risk cases to tertiary care hospitals will help to improve neonatal outcomes.
Downloads
References
Bhutta ZA, Black RE. Global maternal, newborn, and child health— so near and yet so far. N Engl J Med 2013;369:2226-35.
Oestergaard MZ, Inove M, Yoshida S, Mahanani WR, Gore FM,Cousins S, et al. United Nations Inter-Agency Group for Child Mortality Estimation and the Child Health Epidemiology Reference Group. Neonatal mortality levels for 193 countries in 2009 with trends since 1990: A systematic analysis of progress, projections, and priorities. PLoS Med 2011;8:e1001080.
Shiffman J. Issue attention in global health: The case of newborn survival. Lancet 2010;375:2045-9.
South Africa Every Death Counts Writing Group, Bradshaw D, Chopra M, Kerber K, Lawn JE, Bamford L, Moodley J, et al. Every death counts: Use of mortality audit data for decision making to save the lives of mothers, babies, and children in South Africa. Lancet. 2008;12:1294-304.
Elhassan M, Elhassan L, Hassanb A, Mirghani OA, Adam I. Morbidity and mortality pattern of neonates admitted into nursery unit in Wad Medani Hospital, Sudan. Sudan JMS 2010;1:13-5.
Prasad V, Singh N. causes of morbidity and mortality in neonates admitted in Government Medical College, Haldwani in Kumaun region (Uttarakhand) India. JPBS 2011;8:1-4.
Bhutta ZA. Priorities in newborn management and development of clinical neonatology in Pakistan. J Coll Phys Surg Pak 1997;7:231-4.
NFHS-3: Ministry of Health and Family Welfare, Government of India. Available from: http://www.mohfw.nic.in/NFHS-PRESENTATION.htm. [Last accessed on 2014 Nov 08].
Roy KK, Baruah J, Kumar S, Malhotra N, Deorari AK, Sharma JB. Maternal antenatal profi le and immediate neonatal outcome in VLBW and ELBW babies. Indian J Pediatr 2006;73:669-73.
Lawn JE, Cousens S, Zupan J; Lancet Neonatal Survival Steering Team. 4 million neonatal deaths: When? Where? Why? Lancet 2005;365:891-900.
Ng PC. Diagnostic members of infection in neonates. Arch Dis Child 2004;89:229-35.
Roy RN, Nandy S, Shrivastava P, Chakraborty A, Dasgupta M, Kundu TK. Mortality pattern of hospitalized children in a tertiary care hospital of Kolkata. Indian J Community Med 2008;33:187-9.
Garg P, Krishak R, Shukla DK. NICU in a community level hospital. Indian J Pediatr 2005;72:27-30.
UNICEF. The State of The World’s Children, 2010. New York: UNICEF; 2010. p. 92-5.
Gauchan E, Basnet S, Koirala DP, Rao KS. Clinical profi le and outcome of babies admitted to Neonatal Intensive Care Unit (NICU). J Inst Med 2011;33:1-5.
Morbidity and mortality among outborn neonates at 10 tertiary care institutions in India during the year 2000. J Trop Pediatr 2004;50:170-4.
Chandra S, Ramji S, Thirupuram S. Perinatal asphyxia: Multivariate analysis of risk factors in hospital births. Indian Pediatr 1997;34:206-12.
Rakholia R, Rawat V, Bano M, Singh G. Neonatal morbidity and mortality of sick newborns admitted in a teaching hospital of Uttarakhand. CHRISMED J Health Res 2014;1:228-34.
Rashid A, Ferdous S, Chowdhury T, Rahman F. The morbidity pattern and the hospital outcome of the neonates who were admitted in a tertiary level hospital in Bangladesh. Bangladesh J Child Health 2003;27:10-3.
ICMR Young Infant Study Group. Age profi le of neonatal deaths. Indian Pediatr 2008;45:991-4.
Augustine T, Bhatia BD. Early neonatal morbidity and mortality pattern in hospitalised children. Indian J Matern Child Health 1994;5:17-9.
Copyright (c) 2021 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


