The early indicator of significant hyperbilirubinemia in healthy full-term infants at 72 hrs of age: A prospective cohort study
Abstract
Introduction Hyperbilirubinaemia is a very common and frequently benign condition in newborns, but is a leading cause of hospitalisation in the first week of life. Many healthy full-term newborns develop significant hyperbilirubinemia, often leading to serious complications as bilirubin encephalopathy and death. The present study was aimed to determine early predators and risk factors in full-term healthy newborns developing significant hyperbilirubinemia.
Methods - This was a prospective observa-tional cohort study conducted at the department of pediatrics at a tertiary care teaching hospital over 1 year enrolling 200 full-term healthy newborns and following them from birth to 72 hrs of life to determine early predictors of hyperbilirubinemia. The data were analysed using the Statistical Package of Social Science Software (SPSS) program. Bilirubin levels measured at 72 hrs were compared to identify significant hyperbilirubinemia using cut off at or above high intermediate risk zone in Bhutani nom-ogram.
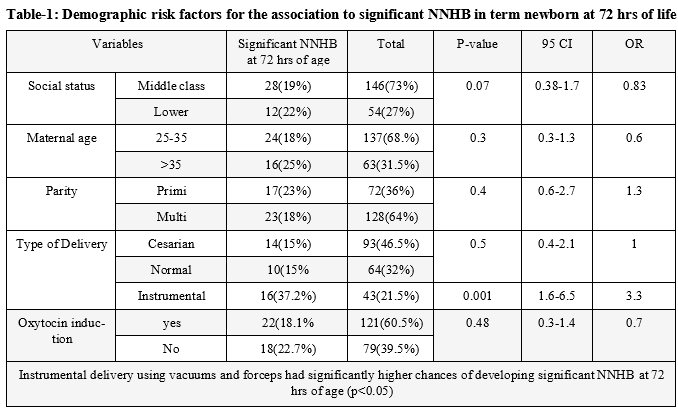
Results- Neonates with birth weight <2.5 kg, born through instrumental delivery, delayed feeding, dehydration, 24 Hr serum bilirubin >6mg/dl and 48 Hr serum bilirubin >11 mg/dl were significantly associated with significant hyperbilirubinemia( p<0.05)
Conclusion- These risk factors can be used as risk indicator to predict the development of significant hyperbiliru-binemia in such newborns and better pre-discharge counselling and followup can be ensured in such newborns especially in re-source-limited settings.
Downloads
References
Olusanya BO, Kaplan M, Hansen TWR. Neonatal hyperbilirubinaemia: a global perspective. Lancet Child Adolesc Health. 2018 Aug;2(8):610-620. doi: 10.1016/S2352-4642(18)30139-1.
Olusanya BO, Osibanjo FB, Slusher TM. Risk factors for severe neonatal hyperbilirubinemia in low and middle-income coun-tries: a systematic review and meta-analysis. PLoS One. 2015 Feb 12;10(2):e0117229. doi: 10.1371/journal.pone.0117229.
Hansen TW. Prevention of neurodevelopmental sequelae of jaundice in the newborn. Dev Med Child Neurol. 2011 Sep;53 Suppl 4:24-8. doi: 10.1111/j.1469-8749.2011.04059.x.
American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics. 2004 Jul;114(1):297-316. doi: 10.1542/peds.114.1.297. Erratum in: Pediatrics. 2004 Oct;114(4):1138.
Murki S, Kumar P, Majumdar S, Marwaha N, Narang A. Risk factors for kernicterus in term babies with non-hemolytic jaun-dice. Indian Pediatr. 2001 Jul;38(7):757-62.
Chawla D, Jain S, Dhir S, Rani S. Risk assessment strategy for prediction of pathological hyperbilirubinemia in neonates. In-dian J Pediatr. 2012 Feb;79(2):198-201. doi: 10.1007/s12098-011-0409-x.
Zimmerman DR, Klinger G, Merlob P. Early discharge after delivery. A study of safety and risk factors. ScientificWorldJour-nal. 2003 Dec 18;3:1363-9. doi: 10.1100/tsw.2003.108.
Bhutani VK, Johnson L, Sivieri EM. Predictive ability of a predischarge hour-specific serum bilirubin for subsequent significant hyperbilirubinemia in healthy term and near-term newborns. Pediatrics. 1999 Jan;103(1):6-14. doi: 10.1542/peds.103.1.6.
Nelson D, Porta R, Blair K, Carter P, Martin M. The duodenal switch for morbid obesity: modification of cardiovascular risk markers compared with standard bariatric surgeries. Am J Surg. 2012 May;203(5):603-608. doi: 10.1016/j.amjsurg.2011.12.004.
Bhutani VK, Johnson LH, Keren R. Diagnosis and management of hyperbilirubinemia in the term neonate: for a safer first week. Pediatr Clin North Am. 2004 Aug;51(4):843-61, vii. doi: 10.1016/j.pcl.2004.03.011.
Adebami, Olusegun J. "Factors associated with the incidence of acute bilirubin encephalopathy in Nigerian population." Journal of Pediatric Neurology 9.03 (2011): 347-353.
Olusanya BO, Akande AA, Emokpae A, Olowe SA. Infants with severe neonatal jaundice in Lagos, Nigeria: incidence, correlates and hearing screening outcomes. Trop Med Int Health. 2009 Mar;14(3):301-10. doi: 10.1111/j.1365-3156.2009.02223.x.
Ameh N, Ameh EA. Timing of passage of first meconium and stooling pattern in normal Nigerian newborns. Ann Trop Paediatr. 2009 Jun;29(2):129-33. doi: 10.1179/146532809X440743.
Gärtner U, Goeser T, Wolkoff AW. Effect of fasting on the uptake of bilirubin and sulfobromophthalein by the isolated perfused rat liver. Gastroenterology. 1997 Nov;113(5):1707-13. doi: 10.1053/gast.1997.v113.pm9352876.
Alex M, Gallant DP. Toward understanding the connections between infant jaundice and infant feeding. J Pediatr Nurs. 2008 Dec;23(6):429-38. doi: 10.1016/j.pedn.2007.12.002.
Siyah Bilgin, B., Altun Koroglu, O., Yalaz, M., Karaman, S., & Kultursay, N. (2013). Factors affecting bilirubin levels during first 48 hours of life in healthy infants. BioMed research international, 2013.
International Volume 2013, Article ID 316430, 6 pages http://dx.doi.org/10.1155/2013/316430.
Tiwari PK, Bhutada A, Agarwal R, Basu S, Raman R, Kumar A. UGT1A1 gene variants and clinical risk factors modulate hyperbilirubinemia risk in newborns. J Perinatol. 2014 Feb;34(2):120-4. doi: 10.1038/jp.2013.140.
Gale R, Seidman DS, Dollberg S, Stevenson DK. Epidemiology of neonatal jaundice in the Jerusalem population. J Pediatr Gastroenterol Nutr. 1990 Jan;10(1):82-6. doi: 10.1097/00005176-199001000-00016.
Alkan S, Tiraş U, Dallar Y, Sunay D. Effect of anaesthetic agents administered to the mothers on transcutaneous bilirubin levels in the neonates. Acta Paediatr. 2010 Jul;99(7):993-6. doi: 10.1111/j.1651-2227.2010.01761.x.
Patil, S. S., Manjunatha, S., Veena, H. C., & Vinod, W. (2015). O xytocininducedneonata l hyperbilirubinemia. Journal of Evidence Based Medicine and Healthcare, 2(21), 3098-3103.
Randev S, Grover N. Predicting neonatal hyperbilirubinemia using first day serum bilirubin levels. Indian J Pediatr. 2010 Feb;77(2):147-50. doi: 10.1007/s12098-009-0335-3.
Alpay F, Sarici SU, Tosuncuk HD, Serdar MA, Inanç N, Gökçay E. The value of first-day bilirubin measurement in predict-ing the development of significant hyperbilirubinemia in healthy term newborns. Pediatrics. 2000 Aug;106(2):E16. doi: 10.1542/peds.106.2.e16.
Agarwal R, Kaushal M, Aggarwal R, Paul VK, Deorari AK. Early neonatal hyperbilirubinemia using first day serum bilirubin level. Indian Pediatr. 2002 Aug;39(8):724-30.
Vailaya R C G, Aiyer S “Early Prediction of Significant Neonatal Hyperbilirubinemia using Serum Bilirubin Levels in Healthy term & near term Newborns”.J. Pub Health Med Res, 2014;2(1):14-9
Copyright (c) 2021 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


