Bubble CPAP (Continuous Positive airway pressure) therapy as a primary mode of respiratory support in preterm newborns with mild to moderate respiratory distress syndrome
Abstract
Background: Respiratory distress syndrome (RDS) is an important cause of morbidity and mortality in preterm infants. Bubble CPAP when used appropriately, is more cost-effective, non-invasive, requires less training and has a lower risk of complications. However, not all preterm infants with RDS respond to CPAP.
Aims: To study the immediate outcome of preterm infants with mild to moderate respiratory distress syndrome on Bubble CPAP. To study the safety and effectiveness of B-CPAP and to identify the risk factors associated with its failure.
Setting: NICU, Department of pediatrics, Mamata general hospital and medical college, Khammam.
Design- Prospective observational study
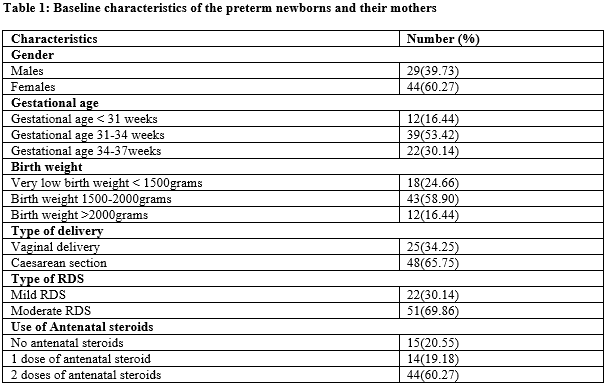
Material and Methods: This duration bound study was conducted from February 2018 to February 2020. Based on the inclusion criteria 73 Preterm babies with mild to moderate respiratory distress syndrome requiring respiratory support were included in this study. Details of birth history, use of antenatal steroids, gestational age, type of delivery, birth weight, Downes score and chest X-ray were recorded. And the effectiveness and outcome of bubble CPAP were studied.
Results: Out of the total of 73 cases, 53(72.60%) were treated successfully, while 20(27.40%) failed bubble CPAP.
Conclusion: Bubble CPAP is the safe primary mode of respiratory support in Preterm newborns with mild to moderate RDS, more effective with early Initiation and in Preterm babies born to mothers with the use of antenatal steroids.
Downloads
References
Singh M. Care of the newborn revised 8thed.CBS Publishers and Distributors Private Limited;2017. p 358
Sahni R. Bubble CPAP: can we predict success or failure? Indian Pediatr. 2010 Feb;47(2):129-30. doi: 10.1007/s13312-010-0019-0.
Van Marter LJ, Allred EN, Pagano M, Sanocka U, Parad R, Moore M, et al. Do clinical markers of barotrauma and oxygen toxicity explain interhospital variation in rates of chronic lung disease? The Neonatology Committee for the Developmental Network. Pediatrics. 2000 Jun;105(6):1194-201. doi: 10.1542/peds.105.6.1194.
Kliegman RM, Stanton BF, Geme JW, Schor NF, Beharman RE. Nelson Textbook of Pediatrics. 19th ed. Elsevier Saunders; 2011. p 585.
Koyamaibole L, Kado J, Qovu JD, Colquhoun S, Duke T. An evaluation of bubble-CPAP in a neonatal unit in a developing country: effective respiratory support that can be applied by nurses. J Trop Pediatr. 2006 Aug;52(4):249-53. doi: 10.1093/tropej/fmi109.
Stevens, T. P., Blennow, M., Myers, E. H., & Soll, R. (2007). Early surfactant administration with brief ventilation vs. selective surfactant and continued mechanical ventilation for preterm infants with or at risk for respiratory distress syndrome. Cochrane Database of Systematic Reviews, (4).
Downes JJ, Vidyasagar D, Boggs TR Jr, Morrow GM 3rd. Respiratory distress syndrome of newborn infants. I. New clinical scoring system (RDS score) with acid--base and blood-gas correlations. Clin Pediatr (Phila). 1970 Jun;9(6):325-31. doi: 10.1177/000992287000900607.
Martin, Richard J., Avroy A. Fanaroff, and Michele C. Walsh, eds. Neonatal-perinatal medicine: diseases of the fetus and infant. Mosby, 2002.
Sankar MJ, Agarwal R, Deorari AK, Paul VK. Sepsis in the newborn. Indian J Pediatr. 2008 Mar;75(3):261-6. doi: 10.1007/s12098-008-0056-z.
Sankar MJ, Sankar J, Agarwal R, Paul VK, Deorari AK. Protocol for administering continuous positive airway pressure in neonates. Indian J Pediatr. 2008 May;75(5):471-8. doi: 10.1007/s12098-008-0074-x.
Koti J, Murki S, Gaddam P, Reddy A, Reddy MD. Bubble CPAP for respiratory distress syndrome in preterm infants. Indian Pediatr. 2010 Feb;47(2):139-43. doi: 10.1007/s13312-010-0021-6.
Urs PS, Khan F, Maiya PP. Bubble CPAP - a primary respiratory support for respiratory distress syndrome in newborns. Indian Pediatr. 2009 May;46(5):409-11.
Sethi A, Mehta NJ, Surti BM, Gamit D, Tada N. Safety and effectiveness of bubble continuous positive airway pressure in neonates with respiratory distress and its failure factors. National Journal of Medical Research. 2015;5(3):202-6.
Boo NY, Zuraidah AL, Lim NL, Zulfiqar MA. Predictors of failure of nasal continuous positive airway pressure in treatment of preterm infants with respiratory distress syndrome. J Trop Pediatr. 2000 Jun;46(3):172-5. doi: 10.1093/tropej/46.3.172.
Sandri F, Ancora G, Lanzoni A, Tagliabue P, Colnaghi M, Ventura ML, Rinaldi M, Mondello I, Gancia P, Salvioli GP, Orzalesi M, Mosca F. Prophylactic nasal continuous positive airways pressure in newborns of 28-31 weeks gestation: multicentre randomised controlled clinical trial. Arch Dis Child Fetal Neonatal Ed. 2004 Sep;89(5):F394-8. doi: 10.1136/adc.2003.037010.
Parasuramappa H, Belavadi G. A descriptive study on the use of bubble CPAP in a level 2 neonatal intensive care unit in Bangalore, India. Sri Lanka Journal of Child Health. 2017 Sep 5;46(3):211-7. Available from: http://doi.org/10.4038/sljch.v46i3.8319
Copyright (c) 2021 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


