Clinical biochemical and serological profile in Children with Celiac disease
Abstract
Background: Celiac disease (CD) is a chronic, immunologically determined form of enteropathy affecting the small intestine, precipitated by the ingestion of gluten-containing foods such as wheat rye, barley etc. This study was taken up to analyze clinical manifestations and biochemical profile of children with celiac disease presenting at KEM Hospital Pune.
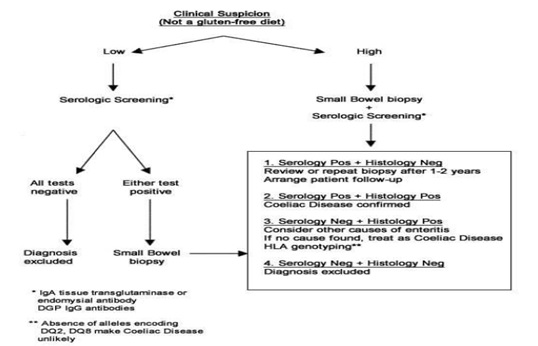
Methods: All children diagnosed as CD in last 5 years and newly diagnosed patients of celiac satisfying inclusion criteria for next 1 year. This is an observational descriptive prospective and retrospective study. CD was diagnosed based on positive tTGA & duodenal biopsy in children with chronic diarrhea & other suggestive features. Hospital records were reviewed for complete follow up data.
Results: In a study period of 12 months we diagnosed 19 children with Celiac Disease, who were studied prospectively, whereas 31 patients who were diagnosed within the last 6 years & were on regular follow up in OPD were studied retrospectively. In the total group of 50 patients in the age range of 1year to 15 years. The presenting clinical features of our group of patients were: chronic diarrhea (92 %), failure to thrive (86%), abdominal pain (34%), abdominal distention (26%), anorexia/vomiting (8%/ 20%), & weight loss (8%). Rare features were fever, fatigue, blood in stools & constipation. In our study anemia was seen in 76% of patients, 58% of prospective patients had low ferritin levels.
Conclusions: In a study period of 12 months we diagnosed 19 children with Celiac disease which goes to go prove that Celiac Disease, is not rare in western Maharashtra. Most patients belonged to the age group 1-5 years (50%) and the majority of patients were females (56%). Chronic diarrhea was the most common presenting complaint in all age groups ( 92%) followed by failure to thrive, not gaining weight and abdominal pain. Constipation was least common. Anemia was the most common laboratory-confirmed finding and the most common type of anemia was iron deficiency anemia. Prevalence Anemia was most common in below 5 yrs.
Downloads
References
Ludvigsson JF, Leffler DA, Bai JC, Biagi F, Fasano A, Green PH, et al. The Oslo definitions for coeliac disease and related terms. Gut. 2013 Jan;62(1):43-52. doi: 10.1136/gutjnl-2011-301346.
Lionetti E, Catassi C. New clues in celiac disease epidemiology, pathogenesis, clinical manifestations, and treatment. Int Rev Immunol. 2011 Aug;30(4):219-31. doi: 10.3109/08830185.2011.602443.
Sood A, Midha V, Sood N, Kaushal V, Puri H. Increasing incidence of celiac disease in India. Am J Gastroenterol. 2001 Sep;96(9):2804-5. doi: 10.1111/j.1572-0241.2001.04150.x.
Sood A, Midha V, Sood N, Avasthi G, Sehgal A. Prevalence of celiac disease among school children in Punjab, North India. J Gastroenterol Hepatol. 2006 Oct;21(10):1622-5. doi: 10.1111/j.1440-1746.2006.04281.x.
Wingren CJ, Agardh D, Merlo J. Sex differences in coeliac disease risk: a Swedish sibling design study. Dig Liver Dis. 2012 Nov;44(11):909-13. doi: 10.1016/j.dld.2012.06.016.
Ivarsson A, Persson LA, Nyström L, Hernell O. The Swedish coeliac disease epidemic with a prevailing twofold higher risk in girls compared to boys may reflect gender specific risk factors. Eur J Epidemiol. 2003;18(7):677-84. doi: 10.1023/a:1024873630588.
Ivarsson A, Hernell O, Stenlund H, Persson LA. Breast-feeding protects against celiac disease. Am J Clin Nutr. 2002 May;75(5):914-21. doi: 10.1093/ajcn/75.5.914.
Myléus A, Hernell O, Gothefors L, Hammarström ML, Persson LÅ, Stenlund H, Ivarsson A. Early infections are associated with increased risk for celiac disease: an incident case-referent study. BMC Pediatr. 2012 Dec 19;12:194. doi: 10.1186/1471-2431-12-194.
Ludvigsson JF, Ansved P, Fälth-Magnusson K, Hammersjö JA, Johansson C, Edvardsson S, Ljungkrantz M, Stenhammar L, Ludvigsson J. Symptoms and signs have changed in Swedish children with coeliac disease. J Pediatr Gastroenterol Nutr. 2004 Feb;38(2):181-6. doi: 10.1097/00005176-200402000-00015.
Fasano A. Clinical presentation of celiac disease in the pediatric population. Gastroenterology. 2005 Apr;128(4 Suppl 1):S68-73. doi: 10.1053/j.gastro.2005.02.015.
McGowan KE, Castiglione DA, Butzner JD. The changing face of childhood celiac disease in north america: impact of serological testing. Pediatrics. 2009 Dec;124(6):1572-8. doi: 10.1542/peds.2008-2373.
Husby S, Koletzko S, Korponay-Szabó IR, Mearin ML, Phillips A, Shamir R, et al. European Society for Pediatric Gastroenterology, Hepatology, and Nutrition. European Society for Pediatric Gastroenterology, Hepatology, and Nutrition guidelines for the diagnosis of coeliac disease. J Pediatr Gastroenterol Nutr. 2012 Jan;54(1):136-60. doi: 10.1097/MPG.0b013e31821a23d0.
Holtmeier W, Caspary WF. Celiac disease. Orphanet J Rare Dis. 2006 Mar 1;1:3. doi: 10.1186/1750-1172-1-3. PMID: 16722573;
Marsh MN. Gluten, major histocompatibility complex, and the small intestine. A molecular and immunobiologic approach to the spectrum of gluten sensitivity ('celiac sprue'). Gastroenterology. 1992 Jan;102(1):330-54.
Sood A, Midha V, Sood N, Kaushal V, Puri H. Increasing incidence of celiac disease in India. Am J Gastroenterol. 2001 Sep;96(9):2804-5. doi: 10.1111/j.1572-0241.2001.04150.x.
Worwood, M. "Indicators of the iron status of populations: ferritin." Assessing the iron status of populations: report of a joint World Health Organization/Centers for Disease Control and Prevention technical consultation on the assessment of iron status at the population level 2 (2007): 35-74.
Stone ML, Bohane TD, Whitten KE, Tobias VH, Day AS. Age related clinical features of childhood coeliac disease in Australia. BMC Pediatr. 2005 May 21;5(1):11. doi: 10.1186/1471-2431-5-11.
Tanpowpong P, Broder-Fingert S, Katz AJ, Camargo CA Jr. Age-related patterns in clinical presentations and gluten-related issues among children and adolescents with celiac disease. Clin Transl Gastroenterol. 2012 Feb 16;3(2):e9. doi: 10.1038/ctg.2012.4.
Wingren CJ, Agardh D, Merlo J. Sex differences in coeliac disease risk: a Swedish sibling design study. Dig Liver Dis. 2012 Nov;44(11):909-13. doi: 10.1016/j.dld.2012.06.016.
Whitacre CC, Reingold SC, O'Looney PA. A gender gap in autoimmunity. Science. 1999 Feb 26;283(5406):1277-8. doi: 10.1126/science.283.5406.1277.
Nussinovitch U, Shoenfeld Y. The role of gender and organ specific autoimmunity. Autoimmun Rev. 2012 May;11(6-7):A377-85. doi: 10.1016/j.autrev.2011.11.001.
Mohindra S, Yachha SK, Srivastava A, Krishnani N, Aggarwal R, Ghoshal UC, et al. Coeliac disease in Indian children: assessment of clinical, nutritional and pathologic characteristics. J Health Popul Nutr. 2001 Sep;19(3):204-8.
Mohandas KM. Surveillance of Indians with liver cirrhosis for treatable hepatocellular carcinoma: another enigma. Indian J Gastroenterol. 2007 Nov-Dec;26(6):261-4.
Rashid M, Cranney A, Zarkadas M, Graham ID, Switzer C, Case S, Molloy M, Warren RE, Burrows V, Butzner JD. Celiac disease: evaluation of the diagnosis and dietary compliance in Canadian children. Pediatrics. 2005 Dec;116(6):e754-9. doi: 10.1542/peds.2005-0904.
Fasano A, Catassi C. Current approaches to diagnosis and treatment of celiac disease: an evolving spectrum. Gastroenterology. 2001 Feb;120(3):636-51. doi: 10.1053/gast.2001.22123.
Villanueva J, Maranda L, Nwosu BU. Is vitamin D deficiency a feature of pediatric celiac disease? J Pediatr Endocrinol Metab. 2012;25(5-6):607-10. doi: 10.1515/jpem-2012-0048.
Riccabona M, Rossipal E. Bedeutung der Sonographie in der Diagnostik der Zöliakie [Value of ultrasound in diagnosis of celiac disease]. Ultraschall Med. 1996 Feb;17(1):31-3. German. doi: 10.1055/s-2007-1000451.
Dogan, G., Ayhan, S., Yilmaz, B., Appak, Y. Ç., Dündar, P. E., Ecemis, T., ... & Kasirga, E. (2015). Relationship Between Duodenal Histopathology and Strong Positive Tissue Transglutaminase Antibodies in Children with Celiac Disease. Güncel Pediatri, 13(3).
Copyright (c) 2021 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


