To study the outcome of exchange transfusion in severe neonatal sepsis in neonates admitted in NICU at Dr. Bhim Rao Ambedkar memorial hospital, Raipur, Chhattisgarh, India
Abstract
Background: Sepsis is one of the most common causes of neonatal mortality and morbidity. Immaturity of the immune system, newborn infants are highly susceptible to systemic infection. Blood exchange transfusion in severe neonatal sepsis remove bacteria, bacterial toxins, and circulating pro-inflammatory cytokines, improve perfusion and tissue oxygenation, correct the plasma coagulation system and enhance immunological defence mechanisms.
Material and methods: This is a hospital-based, time-bound, analytical observational study conducted from January 2019 to December 2019 in the NICU of Dr. B.R.A.M. Hospital & Pt. J. N. M. Medical College, Raipur, Chhattisgarh, India. The data was collected in pre-designed proforma, entered in Microsoft Excel and analysis was done using SSPS v 22.0.
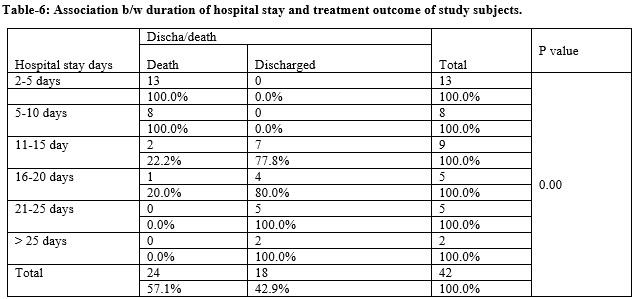
Result: About 42 neonates were diagnosed with severe neonatal severe. Of which 23 (54.76%) were preterm, 42.24% were term neonates. Maximum 22 (52.38%) were VLBW, 4.76% were LBW and 19.05% were with normal birth weight. In the study two-third of 28 (66.67%) were outborn and one third were inborn. In the present study majority of 30 (71.43%) had EOS and 12 (28.57%) had LOS. In our study out of 42 study subjects 24 (57.14%) died and 18 (42.86%) were discharged after blood exchange transfusion. Of those who died 15 (62.5%) were preterm and of those discharged 10 (55.6%) were term neonates (p=0.349). Outborn neonates more died as compare to inborn though this was also not significant (p=0.133). In our study maximum 32 (76.19%) had cardiovascular dysfunction, 28 (66.67%) had respiratory system dysfunction and 11 (26.19%) had renal system dysfunction.
Conclusion: significant reduction of mortality in patients who underwent exchange transfusion, together with the no adverse effects observed, suggest that this procedure should be considered for the treatment of neonates with severe sepsis.
Downloads
References
Liu L, Oza S, Hogan D, Chu Y, Perin J, Zhu J, et al. Global, regional, and national causes of under-5 mortality in 2000-15: an updated systematic analysis with implications for the Sustainable Development Goals. Lancet. 2016 Dec 17;388(10063):3027-3035. doi: 10.1016/S0140-6736(16)31593-8.
Liu L, Johnson HL, Cousens S, Perin J, Scott S, Lawn JE, et al. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet. 2012 Jun 9;379(9832):2151-61. doi: 10.1016/S0140-6736(12)60560-1.
Adkins B, Leclerc C, Marshall-Clarke S. Neonatal adaptive immunity comes of age. Nat Rev Immunol. 2004 Jul;4(7):553-64. doi: 10.1038/nri1394.
Kapur R, Yoder MC, Polin RA. Developmental immunology. In: Fanaroff AA, Martin RJ editor(s). Neonatal-Perinatal Medicine: Diseases of the Fetus and Infant.7th Edition. St Louis: Mosby, 2002.
Levy O. Innate immunity of the newborn: basic mechanisms and clinical correlates. Nat Rev Immunol. 2007 May;7(5):379-90. doi: 10.1038/nri2075.
Wynn J, Cornell TT, Wong HR, Shanley TP, Wheeler DS. The host response to sepsis and developmental impact. Pediatrics. 2010 May;125(5):1031-41. doi: 10.1542/peds.2009-3301.
Shane AL, Stoll BJ. Neonatal sepsis: progress towards improved outcomes. J Infect. 2014 Jan;68 Suppl 1:S24-32. doi: 10.1016/j.jinf.2013.09.011.
Klinger G, Levy I, Sirota L, Boyko V, Lerner-Geva L, Reichman B; Israel Neonatal Network. Outcome of early-onset sepsis in a national cohort of very low birth weight infants. Pediatrics. 2010 Apr;125(4):e736-40. doi: 10.1542/peds.2009-2017.
Stoll BJ, Hansen NI, Adams-Chapman I, Fanaroff AA, Hintz SR, Vohr B, Higgins RD; National Institute of Child Health and Human Development Neonatal Research Network. Neurodevelopmental and growth impairment among extremely low-birth-weight infants with neonatal infection. JAMA. 2004 Nov 17;292(19):2357-65. doi: 10.1001/jama.292.19.2357. PMID: 15547163.
Kermorvant-Duchemin E, Laborie S, Rabilloud M, Lapillonne A, Claris O. Outcome and prognostic factors in neonates with septic shock. Pediatr Crit Care Med. 2008 Mar;9(2):186-91. doi: 10.1097/PCC.0b013e31816689a8. PMID: 18477932.
Prod'hom LS, Choffat JM, Frenck N, Mazoumi M, Relier JP, Torrado A. Care of the seriously ill neonate with hyaline membrane disease and with sepsis (sclerema neonatorum). Pediatrics. 1974 Feb;53(2):170-81.
Xanthou M, Xypolyta A, Anagnostakis D, Economou-Mavrou C, Matsaniotis N. Exchange transfusion in severe neonatal infection with sclerema. Arch Dis Child. 1975 Nov;50(11):901-2. doi: 10.1136/adc.50.11.901. PMID: 1211965; PMCID: PMC1545707.
Töllner U, Pohlandt F, Heinze F, Henrichs I. Treatment of septicaemia in the newborn infant: choice of initial antimicrobial drugs and the role of exchange transfusion. Acta Paediatr Scand. 1977 Sep;66(5):605-10. doi: 10.1111/j.1651-2227.1977.tb07955.x.
Vain NE, Mazlumian JR, Swarner OW, Cha CC. Role of exchange transfusion in the treatment of severe septicemia. Pediatrics. 1980 Nov;66(5):693-7.
Lemos L. Exchange transfusion in treatment of sepsis. Pediatrics. 1981 Sep;68(3):471-2.
Sadana S, Mathur NB, Thakur A. Exchange transfusion in septic neonates with sclerema: effect on immunoglobulin and complement levels. Indian Pediatr. 1997 Jan;34(1):20-5.
Mathur NB, Subramanian BK, Sharma VK, Puri RK. Exchange transfusion in neutropenic septicemic neonates: effect on granulocyte functions. Acta Paediatr. 1993 Nov;82(11):939-43. doi: 10.1111/j.1651-2227.1993.tb12604.x.
Tarnow-Mordi W, Isaacs D, Dutta S. Adjunctive immunologic interventions in neonatal sepsis. Clin Perinatol. 2010 Jun;37(2):481-99. doi: 10.1016/j.clp.2009.12.002.
Gunes T, Koklu E, Buyukkayhan D, Kurtoglu S, Karakukcu M, Patiroglu T. Exchange transfusion or intravenous immunoglobulin therapy as an adjunct to antibiotics for neonatal sepsis in developing countries: a pilot study. Ann Trop Paediatr. 2006 Mar;26(1):39-42. doi: 10.1179/146532806X90592.
Aradhya AS, Sundaram V, Kumar P, Ganapathy SM, Jain A, Rawat A. Double Volume Exchange Transfusion in Severe Neonatal Sepsis. Indian J Pediatr. 2016 Feb;83(2):107-13. doi: 10.1007/s12098-015-1841-0.
Pugni L, Ronchi A, Bizzarri B, Consonni D, Pietrasanta C, Ghirardi B, et al. Exchange Transfusion in the Treatment of Neonatal Septic Shock: A Ten-Year Experience in a Neonatal Intensive Care Unit. Int J Mol Sci. 2016 May 9;17(5):695. doi: 10.3390/ijms17050695.
Bossi E, Meister B, Pfenninger J. Exchange transfusion for severe neonatal septicemia. Pediatrics. 1981 Jun;67(6):941.
Gross SJ, Filston HC, Anderson JC. Controlled study of treatment for disseminated intravascular coagulation in the neonate. J Pediatr. 1982 Mar;100(3):445-8. doi: 10.1016/s0022-3476(82)80457-5.
Dalvi R, Rao S, Rangnekar J, Fernandez A. Exchange transfusions in neonatal sepsis. Indian Pediatr. 1991 Jan;28(1):39-43.
Sadana S, Mathur NB, Thakur A. Exchange transfusion in septic neonates with sclerema: effect on immunoglobulin and complement levels. Indian Pediatr. 1997 Jan;34(1):20-5.
Verma A, Pandita A, Gupta G, Naranje KM, Singh A. Role of DVET in severe neonatal sepsis in an era of high antibiotic resistance: a retrospective observational study. J Matern Fetal Neonatal Med. 2020 May 27:1-6. doi: 10.1080/14767058.2020.1771303.
Copyright (c) 2021 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


