Evaluation of Thyroid Hormone Levels in Full-Term Neonates Presented with Septic Shock
Abstract
Introduction: The incidence of neonatal sepsis in India is 38 per 1000 live births. Many authors found an association between altered thyroid hormone levels and septic shock in neonates and it may be of prognostic importance in septic shock treatment. This study has been conducted to find the relationship between thyroid profile and septic shock in neonates and also to compare the thyroid profile in survivor and non-survivor groups of septic shock patients.
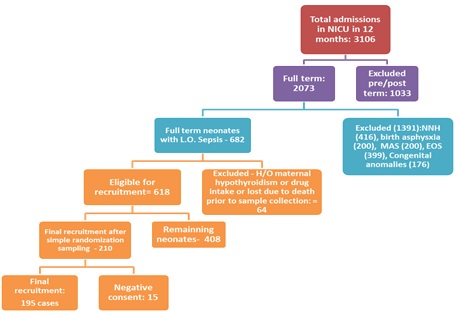
Methods: This analytical prospective cohort study was conducted in the NICU of a tertiary care teaching institution in central India. Full-term neonates with late-onset sepsis were included in this study and estimation of thyroid hormones (TSH, T3, T4, fT3, and fT4) was performed. These neonates were divided into those with and without septic shock patients and levels of thyroid hormones were correlated between these patients to find significant relations. The Vasoactive-Inotropic Score (VIS) score was calculated.
Results: A total of 195 full-term neonates were included in the study. The mean value of TSH, T3, T4, fT3, and fT4 among neonates with septic shock were 5.27 µg/ml, 80.01 ng/dl, 6.36 µg/dl, 1.40 pg/ml, and 1.40 µg/dl, respectively while the values were 5.29 µg/ml, 94.4 ng/dl, 7.25 µg/dl, 1.84 pg/ml, and 1.43 µg/dl, respectively in septic neonates without shock. This difference was statistically significant except for TSH (p>0.05). The mean value of TSH, T3, T4, fT3, and fT4 among septic shock survivors were 5.27 µg/ml, 80.01 ng/dl, 6.36 µg/dl, 1.40 pg/ml, and 1.40 µg/dl and in septic shock non-survivors were 2.40 µg/ml, 37.33 ng/dl, 3.86 µg/dl, 0.99 pg/ml, and 0.84 µg/dl, respectively (p<0.0001). Only T3 was found to be significantly co-related with VIS in septic shock in all the groups (<0.001). The maximum mean value of T3 was observed with VIS less than 20 (84.89 ng/dl) while minimum T3 was observed with VIS more than 50 (35.33 ng/dl).
Conclusion: Our study suggests that TSH, T3, T4, fT3, and fT4 levels are significantly low in patients suffering from the septic shock which may vary in the case of TSH. Also, there is a significant decrease in thyroid profile among septic shock non-survivors as compared to survivors.
Downloads
References
Goldstein B, Giroir B, Randolph A; International Consensus Conference on Pediatric Sepsis. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med. 2005 Jan;6(1):2-8. doi: 10.1097/01.PCC.0000149131.72248.E6.
National neonatal perinatal data base on neonatal sepsis. Available from: www.newbornwhocc.org. Accessed on 28 June 2020
Haque KN. Defining common infections in children and neonates. J Hosp Infect. 2007 Jun;65 Suppl 2:110-4. doi: 10.1016/S0195-6701(07)60026-7.
Calvin B. Williams, Eli M. Eisenstein, and F. Sessions Cole; Immunology and infection; Avery’s Text book diseases of newborn; 992-1017; 9th edition; CristinA.Gleason, Sheri U. Devaskar. Elsevier.
Janet E. Donohue, Sunkyung Yu; hypothalamic-pituitary-adrenal response to critical illness; 1326-1347; Rogers textbook of Pediatrics intensive care; 5th edition.
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M. et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016 Feb 23;315(8):801-10. doi: 10.1001/jama.2016.0287.
McIntosh AM, Tong S, Deakyne SJ, Davidson JA, Scott HF. Validation of the Vasoactive-Inotropic Score in Pediatric Sepsis. Pediatr Crit Care Med. 2017 Aug;18(8):750-757. doi: 10.1097/PCC.0000000000001191.
Gaies MG, Jeffries HE, Niebler RA, Pasquali SK, Donohue JE, Yu S. et al. Vasoactive-inotropic score is associated with outcome after infant cardiac surgery: an analysis from the Pediatric Cardiac Critical Care Consortium and Virtual PICU System Registries. Pediatr Crit Care Med. 2014 Jul;15(6):529-37. doi: 10.1097/PCC.0000000000000153.
Lodha R, Vivekanandhan S, Sarthi M, Arun S, Kabra SK. Thyroid function in children with sepsis and septic shock. Acta Paediatr. 2007 Mar;96(3):406-9. doi: 10.1111/j.1651-2227.2007.00135.x.
Dutta S, Singh S, Bhattacharya A, Venkataseshan S, Kumar P. Relation of Thyroid Hormone Levels with Fluid-Resistant Shock among Preterm Septicemic Neonates. Indian Pediatr. 2017 Feb 15;54(2):121-124. doi: 10.1007/s13312-017-1013-6.
Markus B, Colinus K; Thyroid Gland and Thyroid Hormones; In: Mark A. Sperlings Pediatrics endocrinology.4th edition; Elsevier, 2014: 1167-79
Goldstein B, Giroir B, Randolph A; International Consensus Conference on Pediatric Sepsis. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med. 2005 Jan;6(1):2-8. doi: 10.1097/01.PCC.0000149131.72248.E6.
National neonatology forum guidelines on management of neonatal sepsis. www.nnfpublication.org. (6 May 2020, date last accessed).
Chrousos GP. The hypothalamic-pituitary-adrenal axis and immune-mediated inflammation. N Engl J Med. 1995 May 18;332(20):1351-62. doi: 10.1056/NEJM199505183322008.
Csaba G, Pállinger E. Thyrotropic hormone (TSH) regulation of triiodothyronine (T(3)) concentration in immune cells. Inflamm Res. 2009 Mar;58(3):151-4. doi: 10.1007/s00011-008-8076-8.
Joseph A, Yong Y; Inflammation And Immunity-SIRS, Sepsis, ALI and Multiple organ failure; Text Book of critical pediatrics Fuhrman and Zimmermans; Chapter-6; 5th edition; 1435-1448.
Puopolo KM, Cloherty JP, Eichenwald EC et al. Bacterial and fungal infections. Manual of neonatal care. 2012; 7:624-655.
Donohue JE, Yu S.Hypothalamic-pituitary-adrenal response to critical illness. In: Shaffner DH, Nichols DG (5th). Rogers textbook of Pediatrics intensive care. Lippincott Williams and Wilkins, 2015: 1326-1347.
Williams CB, Eisenstein ME, Cole FS. Immunology and infection In: Gleason CA, Devaskar SU (9th). Avery’s Text book diseases of newborn. Elsevier. 2012: 992-1017
National Family Health Survey-4 by Ministry of health and famiy welfare (NFHS-4) 2015-2016; Madhya Pradesh; MP Fact Sheath 1-4.
Yildizdaş D, Onenli-Mungan N, Yapicioğlu H, Topaloğlu AK, Sertdemir Y, Yüksel B. Thyroid hormone levels and their relationship to survival in children with bacterial sepsis and septic shock. J Pediatr Endocrinol Metab.
Angelousi AG, Karageorgopoulos DE, Kapaskelis AM, Falagas ME. Association between thyroid function tests at baseline and the outcome of patients with sepsis or septic shock: a systematic review. Eur J Endocrinol. 2011 Feb;164(2):147-55. doi: 10.1530/EJE-10-0695.
Borkowski J, Siemiatkowski A, Wołczyński S, Czaban SL, Jedynak M. Ocena wydzielania hormonów tarczycy we wstrzasie septycznym--znaczenie prognostyczne [Assessment of the release of thyroid hormones in septic shock--prognostic significance]. Pol Merkur Lekarski. 2005 Jan;18(103):45-8. Polish.
Zucker AR, Chernow B, Fields AI, Hung W, Burman KD. Thyroid function in critically ill children. J Pediatr. 1985 Oct;107(4):552-4. doi: 10.1016/s0022-3476(85)80017-2.
Starcus N, James Tale; Physiology of Thyroid Gland; Ganong’s review of Medical physiology; 998-1109; 25th edition.
Copyright (c) 2021 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


