Prevalence, Pattern and Outcome of Blood Transfusion: A Private Paediatric Hospital Experience
Abstract
Introduction: Blood transfusion is an essential component of Pediatric care world-wide especially in developing countries. Knowledge about its’ prevalence and pattern is vital in promoting its’ judicious use.
Purpose: To ascertain the prevalence, pattern and outcome of blood transfusion in a private pediatric hospital in south-south Nigeria.
Materials and Methods: A retrospective study was carried out over a 1-year period on children(0-17years) admitted and transfused. Relevant data was retrieved from the hospitals’ Health Management System and analysed.
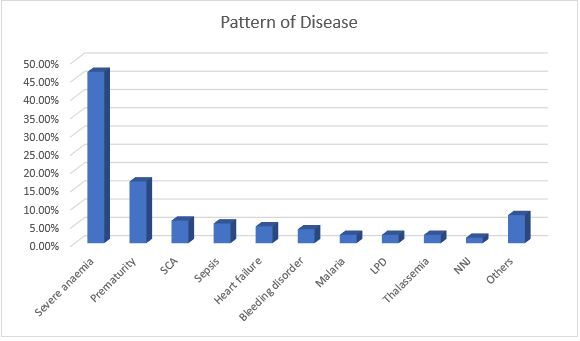
Results: Of 1689 admissions, 69 were transfused giving a prevalence rate of 4.1% with male predominance (M:F ratio of 1.5:1). Eighty-eight blood transfusions were done giving a ratio of 1.3 transfusions/child. Transfused children were mainly 1–12 months of age with mean age of 3.848 ± 4.890months. Most blood transfusions took place within the first 5 hours of prescription and occurred mostly at night. Sedimented cells were mainly used 49(71.0%). Nine(13.0%) children had blood transfusion reactions of which 5(60.0%) had fever. The commonest diagnosis among children transfused were severe anaemia 61(46.9%), prematurity 22(16.9%), sickle cell anaemia 8(6.2%) and sepsis 7(5.4%). Twelve(17.4%) children transfused died. The age of children, type of blood transfused and number of transfusions carried out were significantly associated with the outcome of blood transfusion.
Conclusion: The prevalence of blood transfusion was 4.1%. Commonest diagnosis were severe anaemia, prematurity, sickle cell anaemia and sepsis with mortality rate of 17.4%. It is therefore important to equip private hospitals with functional blood bank services so as to reduce childhood morbidity and mortality.
Downloads
References
2. Ogunlesi TA, Ogunfowora OB. Pattern and determinants of blood transfusion in a Nigerian neonatal unit. Niger J Clin Pract 2011; 14: 354-8.
3. Onyearugha CN, Okoronkwo NC, Onyemachi PE. Blood transfusion: Prevalence, indications and associated factors in children presenting to a tertiary health institution in southeast Nigeria. Amer J Paediatr 2021; 7(2): 53-6. Doi: 10.11648/j.ajp.20210702.13
4. Ogunlesi T, Fetuga B, Olowonyo M, Adekoya A, Adetola O, Ajetunmobi A. Severe childhood anaemia and blood Transfusion in a Nigerian secondary level facility. J Trop Pediatrics, 2016; 62: 107-115. Doi: 10.1093/tropej/fmv083
5. Adegoke S, Ayansanwo A, Oluwayemi I, Okeniyi J. Determinants of mortality in Nigerian children with severe anaemia. South Afr Med J 2010; 102: 807-10
6. Muoneke VU, Ibekwe RC, Nebe-Agumadu HU, Ibe BC. Factors associated with mortality in under-five children with severe anaemia in Ebonyi, Nigeria. Indian Pediatr 2012; 49: 119-23.
7. West BA, Arthur A, Aitafo JE, Onunakwe H. Prevalence, associated factors and outcome of newborns with anaemia as seen in Rivers State University Teaching hospital, Nigeria. ACRI 2021; 21(4): 23-4. Doi: 10.9734/ACRI/2021/v21i430241
8. Muoneke V, Ibekwe R, Nebe-Agumadu H, Ibe B. Severe anaemia in under-five years children in Ebonyi State University Teaching Hospital, Abakaliki. Arch Dis Child 2010; 95: A100-01.
9. Ughasoro MD, Ikefuna AN, Emodi IJ, Ibeziako SN, Nwose SO. Audit of blood transfusion practices in the paediatric medical ward of a tertiary hospital in southeast Nigeria. East Afr Med J. 2013; 90(1): 5-11.
10. Hassell OBI, Maitland K. Blood transfusion in resource-limited settings. In Hunter’s Tropical medicine. 9th ed. London: Magill-Maguire-Ryan-Solomon; 2012: 162-67.
11. McCormick M, Delaney M. Transfusion support: considerations in paediatric populations. Semin Hematol. 2020; 57: 65-72. Doi: 10.1053/j.seminhematol.2020.07.003
12. Shari CR, Sawe HR, Murray BL, Victor MG, Mfinanga JA, Runyon MS. Emergency blood transfusion practices among anaemic children presenting to an urban emergency department of a tertiary hospital in Tanzania. BMC Hematol. 2017; 17:19.
13. Okpe ES, Abok II, Diala UM, Okolo SN, Joseph DE. Indications for Blood Transfusion among Children in a tertiary hospital in north-central Nigeria. J Med Trop 2011; 13 (2): 95-7.
14. Austin NIR, Adikaibe EAB, Ethelbert OO, et al. Prevalence and severity of malaria parasitaemia among children requiring emergency blood transfusion in a tertiary hospital in Imo state, Nigeria. Ann Med Health Sci Res 2014; 4: 619-23.
15. Moncharmont P. Adverse transfusion reactions in transfused children. Transfus Clin Biol. 2019; 26(4): 329-35. Doi: 10.1016/j.tracli.2019.08.002
16. Ino-Ekanem MB, Bassey EU. Overview of blood transfusion in a paediatric medical setting of a tertiary hospital in south-south Nigeria. Inter J Health Sci Res 2016; 6(7): 47-51
17. Guo K, Wang XY, Feng GS, Tian J, Zeng YP, Ma SX, Ni X. The epidemiology of blood transfusion in hospitalized children: A national cross-sectional study in China. Transl Pediatr 2021; 10(4): 1055-1061, doi: 10.21037/tp-20-464
18. Orish VN, Ilechie A, Combey T, Onyeabor OS, Okorie C, Sanyaolu AO. Evaluation of blood transfusions in anemic children in Effia Nkwanta Regional Hospital, Sekondi-Takoradi, Ghana. Am J Trop Med Hyg 2016; 94(3): 691-694, doi: 10:4269/ajtmh.15-0310
19. Goncalez TT, Sabino EC, Capuani L, Liu J, Wright DJ, Walsh JH et al. Blood transfusion utilization and recipient survival at Hospital das Clinicas in Sao Paulo, Brazil. Transfusion 2012; 52(4): 729-738
20. Abhulimhen-Iyoha BI, Isreal-Aina TT. Emergency blood transfusion in children in a tertiary hospital in Nigeria: Indications, frequency and outcome. West Afr J Med 2018; 35(1): 20-24
21. Mosha D, Poulsen A, Reyburn H, Kituma E, Mtei F, Bygbjerg IC. Quality of paediatric blood transfusions in two district hospitals in Tanzania: A cross-sectional hospital based study. BMC Pediatr 2009; 9: 51, doi:10.1186/1471-2431-1189-1151
22. Akodu SO, Adekambi AF, Gbadebo FA, Olanrewaju DM. Indications for blood and blood products transfusions among children in a semi-urban tertiary hospital in Nigeria. Ann Health Res 2020; 6(1): 36-43
23. Ayuketah PO, Tagny CT, Koki NP. Assessment of clinical blood transfusion practice in a pediatric tertiary hospital in Cameroon. J Blood Dis Ther 2019; 1: 101
24. Morley SL, Hudson CL, Llewelyn CA et al. Transfusion in children: Epidemiology and 10-year survival of transfusion recipients. Transfus Med 2016; 26(2): 111-117
25. Slonim AD, Joseph JG, Turenne WM, Sharangpani A, Luban NL. Blood transfusions in children: A multi-institutional analysis of practices and complications. Transfus 2008; 48(1): 73-80, doi: 10.1111/j.1537-2995.2007.01484.x
26. Das Gupta M. Selective discrimination against female children in rural Punjab, India. Popul Dev Rev 1987; 13: 77-100
27. Lozano R, Naghavi M, Foreman KK et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the global burden of disease study 2010. Lancet 2012; 380: 2095-128
28. Fish EN. The X-files in immunity: Sex-based differences predispose immune exposes. Nat Rev Immunol 2008; 8: 737-44
29. Why are Children more vulnerable to resistant infections? News and opinions 2019. Menu ReAct, reactgroup.org
30. World Health Organization. Hospital care for children: Guidelines for the management of common illnesses with limited resources. Geneva: WHO 2005. https://www.who.int/maternal_child_adolescent/documents/9241546700/en/
31. Austin N, Adikaibe E, Ethelbert O et al. Prevalence and severity of malaria parasitaemia among children requiring emergency blood transfusion in a tertiary hospital in Imo State, Nigeria. Ann Med Health Sci Res 2014; 4: 619-623
32. Lashkari C. Anaemia in newborns. News medical life sciences. news-medical.net/health. Cited 12/11/2022
33. Most common blood group in Nigeria + Rarest blood group in Nigeria. nimedhealth.com.ng
34. Ghataliya KJ, Kapadia JD, Desai MK et al. Transfusion-related adverse reactions in pediatric and surgical patients at a tertiary care teaching hospital in India. Asian J Transfus Sci 2017; 11(2): 180-187, doi:10.4103/0973-6247.214348
35. Pedrosa AK, Pinto FJ, Lins LD, Deus GM. Blood transfusion reactions in children: Associated factors. J Pediatr (Rio J) 2013; 89(4): 400-406, doi:10.1016/j.jped.2012.12.009
36. Berg A, Courtney R, Krishnamurti L, Triulzi DJ, Yazer MH. Is intensive monitoring during the first transfusion in paediatric patients necessary? Hematol 2014; 19(5): 304-308, doi:10.1179/16078454137.0000000122
37. Bateman ST, Lacroix J, Boren K, Forbes P, Barton R, Thomas NJ et al. Anemia, blood loss and blood transfusions in North American children in the intensive care unit. Am J Respir Crit Care Med 2008; 178: 26-33
38. Pedro R, Akoch S, Maitland R. Changing trends in blood transfusion in children and neonates admitted in Kilifi district hospital, Kenya. Malar J 2010;9: 300-314
39. Berkley JA, Ross A, Mwang I et al. Prognostic indicators of early and late death in children admitted to district hospital in Kenya: Cohort study. BMJ 2003; 326(7385): 361, doi:10.1136/bmj.326.7385.361
40. English M, Ahmed M, Ngando C et al. Blood transfusion for severe anaemia in children in a Kenyan hospital. Lancet 2002; 359: 494-495
Copyright (c) 2023 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


