Modality of Respiratory Support in Preterm Neonates with Respiratory Distress and its Outcome: Experience of a Tertiary Care Hospital in Bangladesh
Abstract
Background: Preterm neonates are at increased risk of developing respiratory distress after birth. In order to reduce preterm death and their morbidity, identification of etiology and optimum management of respiratory distress is crucial.
Objective: To determine causes of respiratory distress, pattern of respiratory modality used and its outcome among admitted preterm newborns.
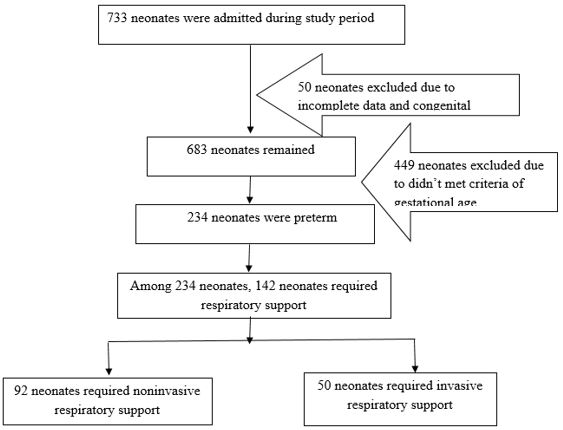
Patients and methods: This study included 142 preterm neonates admitted with respiratory distress and required respiratory support in the NICU of Bangabandhu Sheikh Mujib Medical University, during the period from January 2020 to December 2021. Causes of respiratory distress and pattern of respiratory support was observed. Morbidities and in-hospital mortality were compared between invasive and non-invasive support group in the study.
Results: Mean gestational age among the studied neonates was 32.39 ± 2.46 weeks. Male was predominant (54.2%) and mean birth weight was 1631.44 ± 578.57 g. About 62% belonged to the gestational age within 28 - <34 weeks category. Respiratory distress syndrome (RDS) was the most common cause which was 50.0% following TTN 24.6%, congenital pneumonia 19.0% and PNA 6.3%. Sepsis, septic shock, DIC, NEC and in-hospital mortality, nasal trauma, ROP and IVH occurred significantly higher in the mechanical ventilator support group in comparison to the NIV support group and the p-value were <0.05.
Conclusion: In our study Respiratory distress syndrome is the commonest cause of respiratory distress. Invasive ventilation was associated with significant morbidity and mortality in preterm neonates when compared with those required non-invasive ventilation.
Downloads
References
2. Sweet LR, Keech C, Klein NP, Marshal HS, Tagbo BN, Quine D, et al. Respiratory distress in the neonate: Case definition and Guidelines for data collection, analysis, and presentation of maternal immunization safety data. Vaccine 2017; 35 (48 Pt A): 6506-6517.
3. Ayaz A, Saleem S. Neonatal mortality and prevalence of practices for newborn care in a Squatter Settlement of Karachi, Pakistan: A Cross-Sectional Study. PLOS One 2010; https://doi.org/10.1371/journal.pone.0013783.
4. Bangladesh Demographic and Health Survey 2017–18. Dhaka and Rockville: National Institute of Population Research and Training and ICF; 2020. Available from: https:// dhsprogram .com/ pubs/ pdf/ FR344/ FR344 .pdf [cited 2021 Aug 29].
5. Hong H, Li XX, Li J, Zhang ZQ. High-flow nasal cannula versus nasal continuous positive airway pressure for respiratory support in preterm infants: a meta-analysis of randomized controlled trials. The journal of maternal-fetal & neonatal medicine 2021;34 (2): 259–266.
6. Raju, TNK. Developmental physiology of late and moderate prematurity. Seminars in Fetal and Neonatal Medicine 2012; 17(3), pp. 126–131.
7. Swarnkar K, Swarnkar M. Neonatal respiratory distress in early neonatal period and its outcome. Int J Biomed Adv Res. 2015; 6(9): 643–7.
8. Reuter S, Moser C, Baack M. Respiratory Distress in the Newborn. Pediatrics in Review 2014; 35(10), pp. 417–429.
9. Sharma, P, Poonia A, Bansal R. Comparison of efficacy of nasal continuous positive airway pressure and heated humidified high-flow nasal cannula as a primary mode of respiratory support in preterm infants. Journal of Clinical Neonatology 2019; 8(2), p. 102.
10. Jobe AH. Transition/adaptation in the delivery room and less RDS: “Don’t just do something, stand there!” Journal of Pediatrics 2005; Elsevier: pp. 284–286.
11. Finer N. To intubate or not—that is the question: continuous positive airway pressure versus surfactant and extremely low birthweight infants. Archives of Disease in Childhood. Fetal and Neonatal Edition 2006; 91(6): p. F392-F394.
12. Gomella TL, Cunningham DM, Eyal FG, editors. Neonatology: Management, Procedures, On-call Problems, Diseases and Drugs, Eighth edition. New York. Mc Graw Hill. Lange; 2020.
13. Hedstrom AB, Gove NE, Mayock DE, Batra M. Performance of the Silverman-Andersen Respiratory Severity Score in predicting PCO2 and respiratory support in newborns: a prospective cohort study. Journal of Perinatology 2018; 38: 505-511.
14. Nemr CN, Bakheet MA, Hassan MA. Outcome of neonatal respiratory support modalities in Sohag University Hospital. The Egyptian Journal of Hospital Medicine. 2021; 82 (4): 778-784.
15. Iqbal Q, Younus MM, Ahmed A, Ahmad I, Iqbal J, Charoo BA, et al. Neonatal mechanical ventilation: Indications and outcomes. Indian Journal of Critical Care Medicine. 2015; 19 (9): 27-31.
16. Lategan I, Price C, Rhoda NR, Zar HJ, Tooke L. Respiratory interventions for preterm infants in LMICs: a prospective study from Cape Town, South Africa. Frontiers in Global Women’s Health. 2022; 3: 1-10.
17. Hossain MM, Shirin M, Mamun MA, Hasan MA, Shahidullah M. Predictors of mortality in ventilated neonates in Intensive Care Unit. Bangladesh J Child Health 2009; 33 (3):77-82.
18. Basu B, Sinha SK, Basu T, Mahapatra TKS. Factors predicting mortality in newborn ventilation. Pediatr Pulmonol 2015; 50 (3):271-275.
Copyright (c) 2023 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


