Association of Plasma Lactate Dehydrogenase concentration with Oxygen Dependence in Newborn with Respiratory Distress
Abstract
Background: Newborn with respiratory distress may need only supplemental oxygen, whereas in advance stages may require other respiratory supports like HHFNC, CPAP, MV. Respiratory distress in neonates also showed a relationship between LDH levels and the duration of supplying oxygen. Plasma lactate dehydrogenase (LDH) is an indicator of body tissue hypoxia.
Objectives: To find the association of LDH with a duration of oxygen support among newborns with respiratory distress within 24 hours of life.
Methods: This prospective observational study was carried out on 95 neonates, in the Department of Neonatology, BSMMU, Dhaka from July 2021 to June 2022. Enrolled infants were assigned into three groups: RDS group, TTN group, and congenital pneumonia group. LDH collection was done with all aseptic precautions within 24 hours of admission. Different modes of respiratory support were initiated in patients following NICU protocol according to their respiratory severity score. Respiratory supports were titrated according to the infant’s clinical condition, percent saturation of oxygen, and/or arterial blood gas analysis as per NICU protocol. The primary outcome of the study was the duration of oxygen or respiratory support. All data were recorded in a preformed questionnaire and data were analyzed by statistical package for social sciences (SPSS) version 22.0.
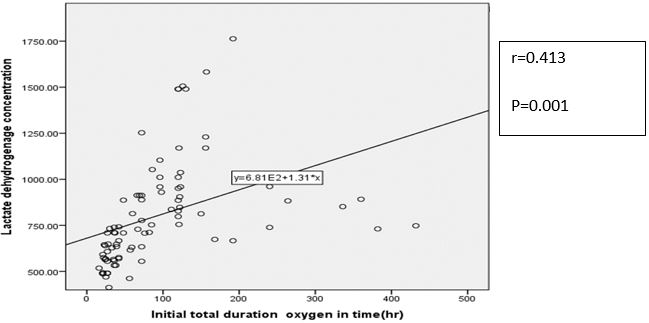
Result: A total of 95 neonates were studied, mean values of LDH among the study groups were 755.64±222.70 u/l, 914.68±304.29 u/l and 742.81±284.70 u/l in TTN, RDS, and congenital pneumonia group respectively. High LDH levels were significantly associated with increased need of oxygen supports in study group (P=0.04). In subgroup analysis showed high LDH was significantly associated with increased need of oxygen support in TTN and congenital pneumonia group (P=0.024, P=0.001) respectively. Pearson correlation showed positive correlation between LDH values and duration of oxygen supports (r=0.413, P=001). In this study, high LDH also significantly associated with high respiratory support (p=0.001). There were no statistical association found in high LDH and hospital stay (P=0.165).
Conclusion: High LDH was associated with the increased need of oxygen and advanced respiratory support among the baby with respiratory distress soon after birth. Also, this study showed a strong association of high LDH with the oxygen duration of TTN and the congenital pneumonia group.
Downloads
References
2. Kommawar,A., 2017.Study of respiratory distress in newborn. Kommawar, A. et al. (2017) ‘Study of respiratory distress in newborn’, International Journal of Contemporary Pediatrics, 4(2), p. 490
3. Ozkiraz S, Gokmen Z, Boke SB, Kilicdag H, Ozel D,and Sert A.,2013.Lactate and lactate dehydrogenase in predicting the severity of transient tachypnea of the newborn’, Journal of Maternal-Fetal and Neonatal Medicine, 26(12), 1245–1248.
4. El Farargy, M. S. and Soliman, N. A.,2017.Early Predictors of Transient Tachypnea of Newborn. Journal of Molecular Biomarkers & Diagnosis. 08(02), 8–11.
5. Jahan, R., 2019. Diagnostic accuracy of lactate dehydrogenase for diagnosis of perinatal asphyxia in neonates with non-reactive CTG’, Pakistan Journal of Medical and Health Sciences, 13(2), pp. 458–460
6. Dave, A., Maru, L. and Jain, A., 2016.LDH (Lactate Dehydrogenase): A Biochemical Marker for the Prediction of Adverse Outcomes in Pre-eclampsia and Eclampsia’, Journal of Obstetrics and Gynecology of India, 66(1), 23–29.
7. Anh, T. N. Van and Hoang, H. H., 2018. The relationship between the plasma lactate dehydrogenase and severe conditions in newborn infant: A prospective study’, Pediatrics & Therapeutics, 08.
8. Elfarargy, M. S. and Al-ashmawy, G. M.,2021. Novel predictor markers for early differentiation between transient tachypnea of newborn and respiratory distress syndrome in neonates.International Journal of Immunopathology and Pharmacology. 35,1-10.
9. Gallacher, D. J., Hart, K. and Kotecha, S., 2016. 27064402’, 12(1), pp. 30–42.
10. Ballard JL, Khoury JC, Wedig K, Wang L, Eilers-Walsman BL, and Lipp R ., 1991.New Ballard Score, expanded to include extremely premature infants. The Journal of Pediatrics, 119,( 3), 417–423.
11. Lackmann, G. M.,1996. Influence of neonatal idiopathic respiratory distress syndrome on serum enzyme activities in premature healthy and asphyxiated newborns. American Journal of Perinatology, 13(6), pp. 329–334
12. Mannan, M.,2018. Neonatal Pneumonia in NICU of a Tertiary Care Center’, Bangladesh Journal of Child Health, 42(3), pp. 112–117.
13. Costa, S. et al., 2012. Transient tachypnea of the newborn and congenital pneumonia: A comparative study’, Journal of Maternal-Fetal and Neonatal Medicine, 25(7), pp. 992–994.
14. An, Y. S.,2014.Serum Enzymes in Predicting Transient Tachypnea of Newborn and Respiratory Distress Syndrome’, Korean Journal of Perinatology, 25(4), p. 284
15. Lee, M , Lee,N , Bae,H, Han,M, Park,H , Byun, Y and Kim,C., 2021.Using lactate dehydrogenase to predict the severity of respiratory distress in term newborn infants with no perinatal asphyxia.Turkish Journal of Pediatrics, 63(3), 393–403
16. Stoicescu, E. R.,2022.The Assessment of COVID-19 Pneumonia in Neonates: Observed by Lung Ultrasound Technique and Correlated with Biomarkers and Symptoms’, Journal of Clinical Medicine, 11(12)
17. Karlsson, M.,2012.Lactate dehydrogenase as an indicator of severe illness in neonatal intensive care patients: A longitudinal cohort study’, Acta Paediatrica, International Journal of Paediatrics, 101(12), pp. 1225–1231
18. Liu Y, Shen Y,and Wei B., 2022 . The Clinical Risk Factors of Adenovirus Pneumonia in Children Based on the Logistic Regression Model: Correlation with Lactate Dehydrogenase. Int J Clin Pract.Vol.2022,1-3
19. Kamath, M. K. Asha,M, Saihari, B and Sneha, M., 2019.Lactate Dehydrogenase as a Prognosticating Tool in Predicting NICU Stay and Oxygen Dependence in Meconium Stained Amniotic Fluid Neonates’, Journal of Clinical and Diagnostic Research, 11–13.
Copyright (c) 2023 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


