Striking the Right Balance: A Review of Pre-procedural Fasting Protocols and their Impact on Pediatric Patients
Abstract
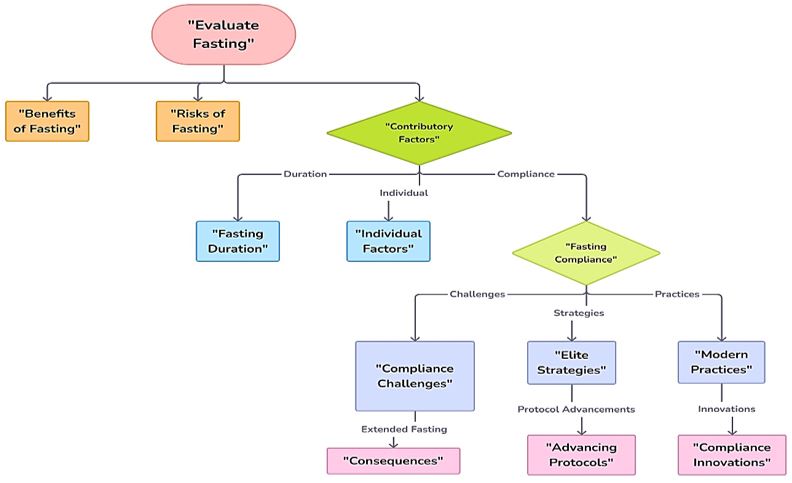
Introduction: Preoperative fasting guidelines have evolved from Sir Joseph Lister's 1883 recommendations to more flexible protocols such as the 1999 American Society of Anaesthesiologists’ 6-4-2 rule and 2022 6-4-1 regimen. Despite these updates, outdated practices still lead to prolonged fasting and related complications. Aim: This scoping review evaluates current preoperative fasting protocols for Pediatric patients, assesses their impact on outcomes, and identifies areas for improvement to balance aspiration risks with the adverse effects of prolonged fasting. Methodology: An orderly search was conducted across PubMed, Scopus, Science Direct, etc., (up to June 10, 2024) using Boolean operators and keywords like "pre-procedural fasting," "protocols," "children," and "influencing factors" to select relevant studies based on inclusion criteria. Results: Prolonged fasting, sometimes up to 16 hours, causes discomfort and increases risks of hypotension, nausea, and hypoglycemia. Challenges include outdated practices, unpredictable surgical schedules, and communication gaps, leading to non-compliance and cancellations. Modern guidelines balance benefits and risks by incorporating a better understanding of gastric emptying and child comfort. Conclusion: Optimizing preoperative fasting for pediatric patients requires flexible protocols, enhanced family education, and improved healthcare team coordination. Continued research and a multidisciplinary approach are essential for refining practices, improving outcomes, and increasing satisfaction.
Downloads
References
2.Pfaff KE, Tumin D, Miller R, Beltran RJ, Tobias JD, Uffman JC. Perioperative aspiration events in children: A report from the Wake Up Safe Collaborative. Pediatr Anesth. 2020 Jun;30(6):660–6.
3. Puri K, Kundal R, Kundal V, Pawar JG, Kumar A, Choudhury SR. Influence of Parental Awareness Drive on Preoperative Fasting Compliance in Pediatric Day Care Surgery. J Indian Assoc Pediatr Surg. 2022;27(2):236–40.
4.Hassouneh O, Al-Oran H, Al-Smadi E, Qzih E. Preoperative fasting among children who undergoing surgery. CHILDS Health. 2023;18(6):474–8.
5.Ricci Z, Colosimo D, Saccarelli L, Pizzo M, Schirru E, Giacalone S, et al. Preoperative clear fluids fasting times in children: retrospective analysis of actual times and complications after the implementation of 1-h clear fasting. J Anesth Analg Crit Care. 2024 Feb 13;4(1):12.
6.Rüggeberg A, Meybohm P, Nickel EA. Preoperative fasting and the risk of pulmonary aspiration-a narrative review of historical concepts, physiological effects, and new perspectives. BJA Open. 2024 Jun;10:100282.
7. Silva Bergantini L, Tsukuda Ichisato SM, Águila Nunes MS, Molena Fernandes CA. Preoperative fasting time in children undergoing elective surgical procedures. Rev Rene. 2021 Jan 1;22(1).
8.Carroll AR, McCoy AB, Modes K, Krehnbrink M, Starnes LS, Frost PA, et al. Decreasing pre-procedural fasting times in hospitalized children. J Hosp Med. 2022 Feb;17(2):96–103.
9.Thomasseau A, Rebollar Y, Dupuis M, Marschal N, Mcheik J, Debaene B, et al. Observance of preoperative clear fluid fasting in pediatric anesthesia: oral and written information versus text message information. A before-and-after study. Paediatr Anaesth. 2021 May;31(5):557–62.
10.Al-Robeye AM, Barnard AN, Bew S. Thirsty work: Exploring children’s experiences of preoperative fasting. Paediatr Anaesth. 2020 Jan;30(1):43–9.
11.Veigaard N, Brahe N, Hansen TG, Clausen NG. Fasting in pediatric anesthesia: the art of making simple things complex. Signa Vitae. 2021;17(5):11–7.
12.Singla K, Bala I, Jain D, Bharti N, Samujh R. Parents’ perception and factors affecting compliance with preoperative fasting instructions in children undergoing day care surgery: A prospective observational study. Indian J Anaesth. 2020 Mar;64(3):210–5.
13.Ghimire A, Maves GS, Kim SS, Raman VT, Tobias JD. Patient Characteristics Associated with NPO (Nil Per Os) Non-Compliance in the Pediatric Surgical Population. Pediatr Health Med Ther. 2022 Jun;Volume 13:235–42.
14.Hajian P, Shabani M, Khanlarzadeh E, Nikooseresht M. The Impact of Preoperative Fasting Duration on Blood Glucose and Hemodynamics in Children. J Diabetes Res. 2020;2020:6725152.
15.Aroonpruksakul N, Punchuklang W, Kasikan K, Laotaweesuk N, Phoson P, Khongrod R, et al. The actual duration of preoperative fasting in pediatric patients, and its effects on hunger and thirst: a prospective observational study. Transl Pediatr. 2023 Feb 28;12(2):146–54.
16.Özdemir Ş, Dolgun E. The effect of preoperative fasting to postoperative agitation, nausea, and vomiting in children with tonsillectomy: The effect of preoperative fasting. Med Sci Discov. 2021;8(6):394–400.
17.Li C, Shao H, Huang S, Zhang T, Su X, Zhu S. Effects of an Individualized Fasting Program on Fasting Time and Comfort in Infants and Young Children During the Perioperative Period. J Perianesth Nurs. 2020 Jun;35(3):326–30.
18.Junior RERS, Soriano C, Lima P, de Oliveira Santos BF, Pereira W, de Brito Filho MT, et al. Beyond Guidelines: The Persistent Challenge of Preoperative Fasting Times. 2023 [cited 2024 Aug 9]; Available from: https://www.preprints.org/manuscript/202310.0743
19.Yimer AH, Haddis L, Abrar M, Seid AM. Adherence to pre-operative fasting guidelines and associated factors among pediatric surgical patients in selected public referral hospitals, Addis Ababa, Ethiopia: Cross sectional study. Ann Med Surg 2012. 2022 Jun;78:103813.
20.Raval MV, Brockel MA, Kolaček S, Simpson KE, Spoede E, Starr KNP, et al. Key Strategies for Optimizing Pediatric Perioperative Nutrition-Insight from a Multidisciplinary Expert Panel. Nutrients. 2023 Mar 3;15(5):1270.
21.Zhang E, Hauser N, Sommerfield A, Sommerfield D, von Ungern-Sternberg BS. A review of pediatric fasting guidelines and strategies to help children manage preoperative fasting. Paediatr Anaesth. 2023 Dec;33(12):1012–9.
22.Assen HE, Hassen AM, Abate A, Liyew B. Preoperative Fasting Time and Its Association with Hypoglycemia during Anesthesia in Pediatric Patients Undergoing Elective Procedures at Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia. BioMed Res Int. 2021;2021:9166603.
Copyright (c) 2024 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


